The MRI Appearance of Anterior Cruciate Ligament Tear

Anterior cruciate ligament (ACL) tears are a frequent reason for ordering knee MRI examinations in the post-traumatic patient. Typically we think about the professional athlete when imagining an ACL tear, but it can happen to anyone. An activity as innocuous as jumping on a backyard trampoline can result in internal knee derangement. ACL tears are found in the young and old alike. MRI is an excellent modality for imaging such tears, and, in fact, is the best modality for this purpose, short of arthroscopy.
The normal ACL as described in a previous article is a thin, somewhat fan-shaped ligament. It runs from the medial aspect of the lateral femoral condyle to the intercondylar region of the tibia adjacent to the tibial spines. It is a low signal intensity structure on both the T-1 and T-2 weighted sequences and can appear somewhat striated (Figure 1). In figure 1, individual intact fibers can be identified as they fan out on the attachment at the tibia. The superior margin of the ligament normally has an angle that approximates the roof of the intercondylar region of the femur, as is also seen in figure 1. An angle that differs from that of the roof can be a secondary indicator of ligament tear.
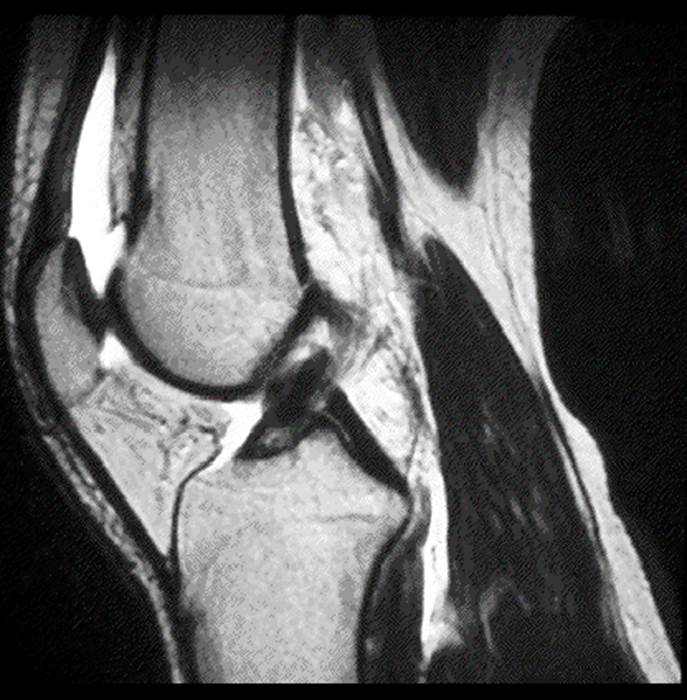
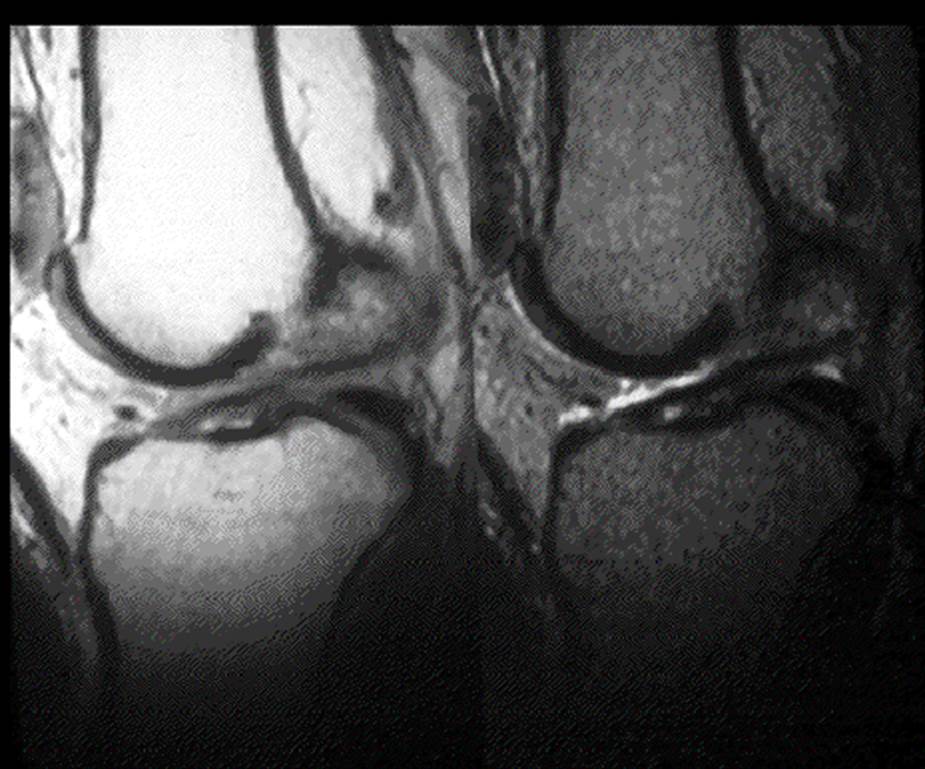
An area of high signal intensity on the sagittal T-2 weighted images (1) within the ligament, usually at the femoral attachment, is a sign of tear (Figure 2). In figure 2, a high signal intensity focus is noted at the proximal attachment on the femur. The apparent absence of the ligament can also be a sign of tear; however, due to the normal thinness of the ligament, it may be possible that the orientation of the slices may cause the cuts to pass to each side of the ligament, rather than through it, on the sagittal cuts. Thus, it may be present and normal, however not be visualized. This problem may be overcome by the use of thin slice imaging through the ACL, which is routinely done at a number of imaging centers. The ACL is probably best seen on the sagittal images, but with experience, it can be identified on the coronal images as well. The coronal images may thus be used to confirm the presence of the ligament if it is not well seen on the sagittal images. Another secondary indicator of ACL tear may be a posterior translation of the femur on the tibia, as the ligament is a primary stabilizer to prevent such motion. In the acute setting, an ACL tear may result in marked bleeding into the joint with a copious joint effusion. These changes are easy to identify on MRI and can be seen on figure 2 as high signal intensity in the suprapatellar pouch anterior to the distal femur on this T-2 weighted image. A ligament that has a horizontal orientation is decidedly torn and this is sometimes referred to as the “laying down sign” (Figure 3). In figure 3 there are two images, a T-1 weighted on the left and a fat-suppressed image on the right. In both, the ACL is visualized as a largely horizontal hypointense line between the femur and the tibia.
In the subacute setting, a large joint effusion may not be present. This should not be a deterrent to suspecting a torn ACL, however. I have seen many ACL tears in which there was little or no joint effusion. Individual ACL fibers should be able to be identified and there should be no areas of increased signal on the T-2 or fat suppressed sequences within the ligament in the intact ACL. Also, always assess the angle of the ligament, as mentioned earlier. In the subacute or chronic setting, this may be our best sign in identifying a tear.
Medial collateral ligament tears are often associated with ACL tears, as are torn medial menisci. This combination of injury is referred to as the triad of O’Donoghue (2). The finding of any of these injuries in the post traumatic setting should be cause for a thorough search of the other related areas.
A comprehensive report of an ACL tear should include the site of the tear, the orientation of the ligament, any associated avulsive osseous injury, as well as the previously described MCL or meniscal injury.
References:
Stoller D. W.: Magnetic Resonance Imaging in Orthopaedics and Sports Medicine, ed 2. Philadelphia, J. B. Lippincott Company 1993.
Yochum T.R., Rowe L.J.: Essentials of Skeletal Radiology, ed 3. Philadelphia, Lippincott Williams & Wilkins, 2005.