Signs and Symptoms of Chondrosarcoma

When I taught radiology, I would often ask the following question of my students; What two things do sharks and chondrosarcoma have in common? Although it would seem incongruous to throw in a subject like sharks with a lecture about primary bone tumors, the answer is quite interesting. Both sharks and chondrosarcomas are composed of cartilage (the shark and ray family of fishes have a cartilaginous skeleton, not a bony one). The second thing they have in common is that both are capable of killing you. Unlike a shark, however, a chondrosarcoma is going to take much longer to kill you. Chondrosarcomas, although malignant neoplasms, vary in their degree of aggressiveness and are the second most common primary malignant tumor of bone (1).
Lesions are graded as follows:
Grade I lesions are considered low grade and are similar to benign cartilage lesions histologically and have a low potential for metastasis.
Grade II lesions are an intermediate grade and approximately 10-15% will metastasize.
Grade III lesions are characterized as high grade and feature a 50% rate of metastasis.
Symptoms
Clinically, chondrosarcomas cause a dull, deep achy type pain. Night pain may be a prominent feature. Pain may be present for up to one year before diagnosis. If near a joint, there may be a limitation of joint motion. Pathologic fractures may occur due to local weakening of the bone.
Radiology
On x-ray, chondrosarcomas are large, generally greater than 5.0 cm. There may be thinning of the cortex with endosteal scalloping. Local bony destruction is seen and varies with the histological grade. Calcifications may be seen within the matrix of the lesion. The appearance of the calcifications has been described by a number of terms, including “stippled,” “punctate,” “popcorn,” and “arc and ring.” A periosteal reaction may be seen in some lesions.
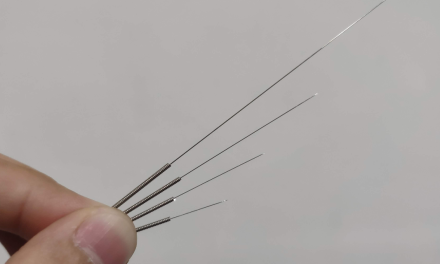
Figure 1 demonstrates a lesion with gross bony expansion in the humeral head. Cortical thinning is present with a violation of the cortex at the medial aspect of the lesion. Calcifications are diffusely noted within the matrix of the lesion. These are all findings consistent with an aggressive bone tumor.
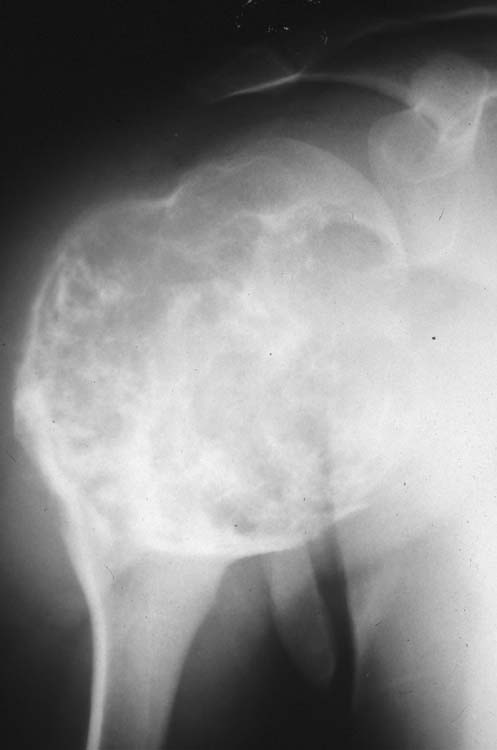
Figure 2 features a very dense lesion with flocculent calcification in the left ilium. The calcification is less dense at the lateral aspect of the lesion. In figure 3 there is a lucent lesion noted in the left femoral neck and intertrochanteric region with dense calcifications in the center.

Figure 2 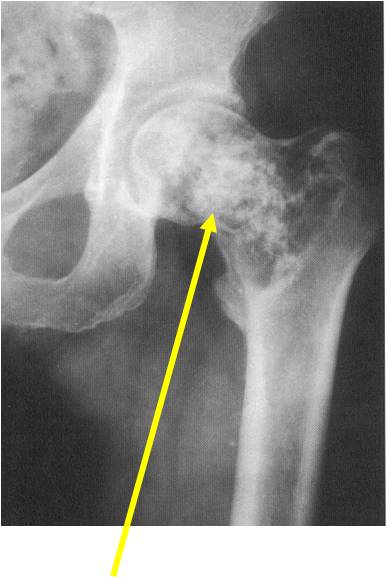
Figure 3
It is possible for benign cartilage lesions, such as enchondromas and osteochondromas, to undergo malignant degeneration, although this is considered uncommon. Generally, the closer a lesion is to the axial skeleton, the greater the likelihood of malignant degeneration.
Signs that a previously benign lesion may be undergoing malignant change include:
– Increase in lesion size;
– A decrease in the density of calcifications within the lesion;
– Erosion of the endosteum;
– Cortical destruction;
– An associated soft tissue mass; and
– Expansion of the cartilage cap in an osteochondroma.
Pain that develops in a previously non-symptomatic cartilaginous lesion may be a clinical symptom of malignant degeneration.
Tumors that may be included in a differential diagnosis include metastatic carcinoma; chondroblastoma; chondroma; chondromyxoid fibroma; fibrosarcoma; fibrous dysplasia; osteosarcoma; and synovial chondromatosis. The relative likelihood of these differentials would, of course, depend on patient age, location of the lesion in the skeleton and location within a particular bone among other variables.
Treatment
The primary treatment for local chondrosarcoma is wide surgical excision, when amenable. This may be feasible for an appendicular location; however, if in the axial skeleton, this is usually not possible, and the prognosis is not as favorable. Chemotherapy and radiation therapy are utilized when surgically inaccessible areas are involved or in cases of metastasis.
Patients with known benign cartilage lesions should be monitored clinically for the advent of pain. It is generally not recommended to monitor benign lesions radiographically.
References:
- Medscape, Chondrosarcoma, Updated: Sep 12, 2016 Author: Palaniappan Lakshmanan, MBBS, MS, AFRCS, FRCS(Tr&Orth); Chief Editor: Harris Gellman, MD