Intersegmental Dysfunction or Mass Lesion

Intersegmental Dysfunction or Mass Lesion
Although the axiom, “When you hear hoofbeats behind, you expect to turn around and see a horse and not a zebra,” is generally true, there are exceptions to all rules. The following is a case study of a patient I encountered recently that is an example of this rule breaking, and it emphasizes the unparalleled role of MRI in the differential diagnosis. In this article, I will review the imaging in this case, because it is quite striking.
A 19-year-old female patient presented to her DC for a complaint of lower back pain. She was a softball pitcher and over the past 4-5 weeks had developed worsening lower back pain. She stated that the pain in her back did not extend into the extremities and that there was no particular physical activity that aggravated the condition. The pain was not more prevalent at any specific time of day. Ibuprofen helped the pain slightly; however, it always came back to the same level. She reported no other health problems.
Examination
Physical examination revealed an apparently healthy, well-nourished 19-year-old female with an appropriate weight for her height. Both orthopedic and neurologic tests were normal:
Plain film x-rays of the lumbar spine were obtained and were interpreted as normal.
Initial Treatment
She was placed on a program of spinal manipulation with a presumptive diagnosis of intersegmental dysfunction of the lumbar spine, and she was advised to refrain from softball participation for the coming 4 weeks. The patient was seen for two weeks at a frequency of 3 times per week. At the end of the second week, there had been no improvement in the lower back pain. Because there had been no positive response to the treatment, the treating physician was suspicious and ordered a non-contrast MRI of the lumbar spine.
Imaging
I have attached the pertinent images from this study. Figure 1 is a non-contrast midsagittal image which reveals an area of altered signal intensity within the spinal canal at the S1 level that extends slightly into the S2 level. There is homogeneously intermediate signal intensity within the thecal sac. Normally this area would exhibit signal intensity continuous with the remainder of the sac, which is hypointense, representing cerebrospinal fluid (CSF). The fat suppressed mid-sagittal image (Fig.2) shows a well-defined area of signal hyperintense to normal CSF. The initial interpretation of the study concluded that there was likely a mass lesion within the spinal canal at the S1-S2 level and suggested intravenous contrast follow-up imaging. A contrast study was performed a week later. Note on the follow-up post contrast T-1 sagittal image (Fig. 3) that there has been a uniform enhancement of the lesion. This indicates that the lesion is in fact solid and not cystic. Possibilities for this appearance include meningioma, schwannoma or perhaps an intradural glial tumor such as ependymoma. The patient was referred to an oncologist for follow-up. A subsequent biopsy of the lesion revealed a myxopapillary ependymoma.

Figure 1 
Figure 2 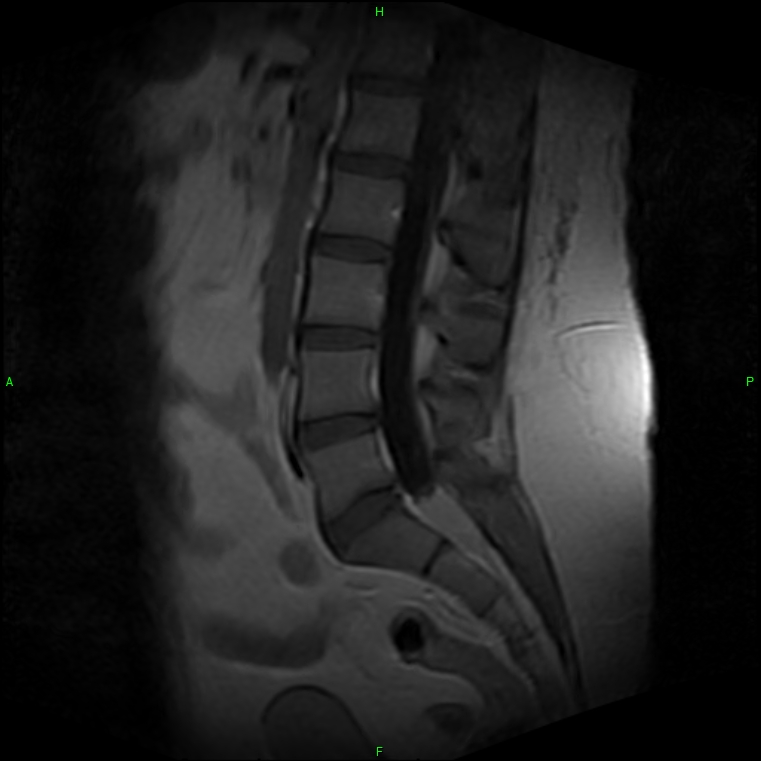
Figure 3
Tumors
The classification of ependymomas includes myxopapillary, subependymomas, ependymomas (grade II) and anaplastic ependymomas (grade III). Both myxopapillary and subependymomas are considered grade I tumors.
The myxopapillary tumors likely arise from the ependymal glial cells of the filum terminale when involving the distal spine. They are considered intradural and extramedullary. Symptoms of lower back pain and lower extremity pain are common. Patient age ranges vary from 6 to 82 years. While this is not a particularly aggressive form of the tumor, recurrence is common, particularly when they are multifocal, large or extend outside the spinal canal. Younger patients tend to have a greater incidence of recurrence. Treatment includes surgery, which is often curative if all the tumor is removed. Often radiation or chemotherapy is utilized as well to help prevent a recurrence. An adjunct therapy is also used in cases in which total resection is not possible.
Conclusion
Follow-up, in this case, is not yet available. The patient had been scheduled for surgery. This case emphasizes the necessity of assiduously evaluating patient response to treatment. If a case is not responding as anticipated, advanced imaging can serve as a valuable tool in assessing a given patient’s condition.