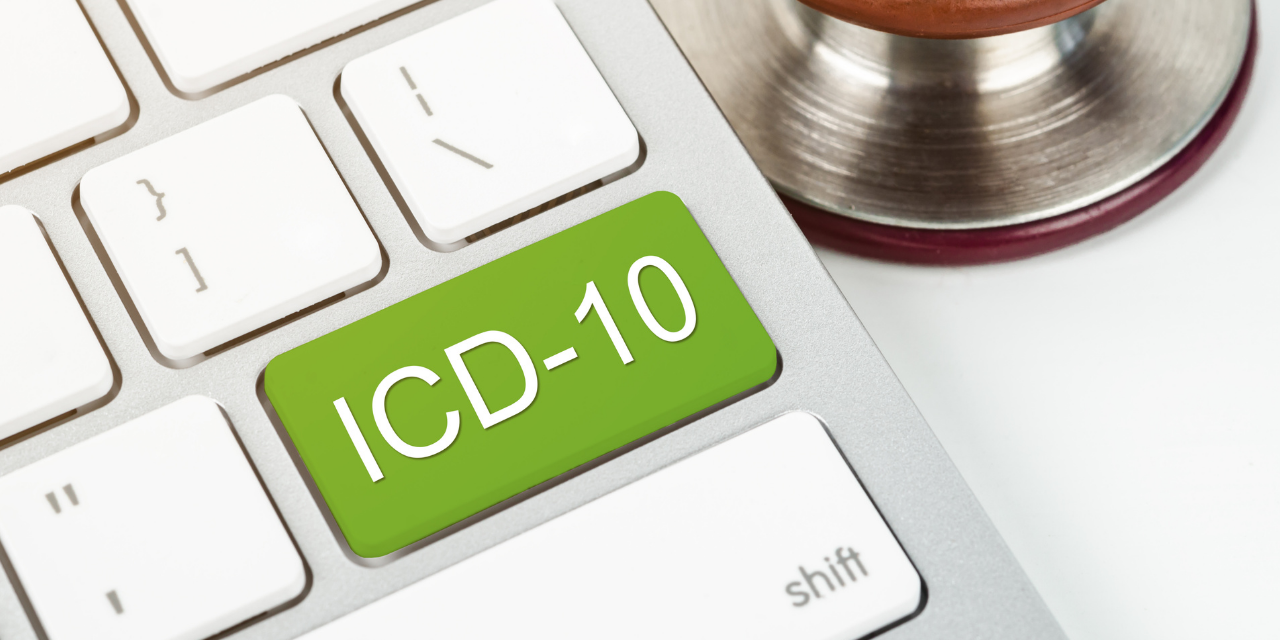
ICD-10 Guidelines and Code Changes Take Effect October 1, 2021
[Editor’s Note: Dr. Mario Fucinari is covering ICD-10 changes and many other key topics as a part of the “Health Care Updates for the Pandemic Era Practice” at the 2021 ICS Virtual Conference this weekend. Find out more here.]
The World Health Organization and the Centers for Medicare and Medicaid Services have released the diagnosis code updates for the fiscal year 2022. The changes in codes and guidelines take effect on October 1, 2021, and affect all services rendered on or that date. Therefore, all offices must be aware of the changes and assess how the changes will impact your office. Ignorance or a lack of action on your part may lead to denials or recoupment.
Unlike FY 2021, there are not as many code changes this year, but the impact may still be the same in your office. 165 new codes have been implemented this year, compared to 485 codes last year.
In addition, there were updates to the ICD-10-CM Official Guidelines for Coding and Reporting. Every physician and their staff should remember that it is imperative to “code to the highest level of specificity.” Insurance carriers base their reimbursement on the codes you list on the claim form. A non-specific code yields limited information and will yield a limited amount of approved treatment. It is essential to review the guidelines and the new codes to ensure you are assigning the most appropriate codes.
Among the notable guideline changes are involving laterality. When the patient’s provider does not document laterality, code assignment for the affected side may be based on medical record documentation from other clinicians. Codes for an “unspecified” side should rarely be used, such as when the documentation in the record is insufficient to determine the affected side, and it is impossible to obtain clarification. Any unspecified code is deemed a red flag in coding. Be specific.
In the past, the provider or their staff had to confirm a condition. The guidelines now state that exceptions will allow the doctor to report information gained from outside records. These would include the following:
- Body Mass Index (BMI)
- Depth of non-pressure chronic ulcers
- Pressure ulcer stage
- Coma scale
- NIH stroke scale (NIHSS)
- Social determinants of health (SDOH)
- Laterality
- Blood alcohol level
The importance of consistent, complete documentation in the patient’s medical record cannot be overemphasized. If it is not documented, it never happened! A resultant policy and procedure should review each chart entry to verify the specific reason for the encounter, the conditions being treated or addressed, and the functional improvements.
Among the 165 code changes for this year, the most impactful changes to our practice involve low back pain and headaches. Low back pain (M54.5) is a broad and non-specific diagnosis. You would never report to a patient in the report of findings that you have determined they have low back pain. It does not tell us why they have low back pain. The codes are also used for tracking purposes, reimbursement policies, and evidence-based practice guidelines. Therefore, beginning October 1, 2021, the low back pain or lumbago code of M54.5 has been deleted and replaced with three other codes.
M54.5 Lumbago/Low Back Pain DELETED
NEW CODES TO CHOOSE FROM INCLUDE:
M54.50 Low back pain, unspecified
M54.51 Vertebrogenic low back pain
M54.59 Other low back pain, not otherwise specified
I would advise the doctor to consider not using M54.50 and M54.59 due to their unspecified nature. However, you may use vertebrogenic low back pain (M54.51) if that is the highest degree of specificity known. If you have a radiology report identifying lumbar degenerative disc disease or spinal stenosis, those would be even more specific than vertebrogenic low back pain. Ask yourself why they have low back pain? That is the code you should be using.
Another significant update is a new code for cervicogenic cephalgia (G44.86). Code the associated cervical spine condition, then the cervicogenic cephalgia. An example would be
Cervical degenerative disc disease M50.32
Cervicaogenic cephalgia G44.86
I think that we can all agree that the Sars-CoV-2 virus, which causes COVID-19, is the most significant pandemic of our lifetime. Not only are we dealing with family, staff, and patients with COVID, but now we are seeing patients come in with sequelae of the virus. The sequelae are known as Long COVID or Long-Haul COVID. Symptoms of Long-Haul COVID include the following:
- Fatigue
- Ataxic gait
- Headaches
- Loss of smell or taste
- Loss of proprioception
- Joint or muscle pain
- Deconditioning
- Chest pain
- A-fib
- Depression
Due to this growing problem, a new Long-Haul COVID (U09.9) code has been assigned for FY 2022 and is considered complicating factor. First, code the specific symptom(s) or condition(s), and as a complicating factor, use the code U09.9, Post COVID-19 condition, unspecified. Additionally, there were updates for numerous other codes for conditions that may be seen in the chiropractic office, such as Sjogen Syndrome, Ankylosing Spondylitis, and Pediatric Feeding Difficulty (PDF). It is recommended that the doctor and staff attend upcoming classes to learn how to code the conditions that matter in the treatment of your patient