
Calcium Pyrophosphate Dihydrite Deposition Disease

Imaging of Calcium Pyrophosphate Dihydrite Deposition Disease
We see degenerative joint disease (DJD) and degenerative disc disease so often on our radiographs that it is tempting to label any joint with decreased joint spacing and osteophyte formation as DJD. Other conditions may precipitate joint changes that mimic those of DJD, however, and it is prudent to recognize these conditions and not simply write off our findings as typical DJD. One of these conditions is calcium pyrophosphate dihydrite crystal deposition disease (CPPD).
CPPD is the most common crystalline induced arthropathy. The male-to-female incidence ratio is about equal. This metabolic arthropathy may result in radiographic findings which are very similar to DJD. Clinically the disease may resemble rheumatoid arthritis, gout or degenerative joint disease. Various manifestations are sometimes referred to as “pseudogout” or “pseudorheumatoid” because of these similarities. Attacks of pain are usually intermittent and may be mono-articular or poly-articular. Symptoms consist of pain, redness, and swelling. Fortunately, there are radiographic findings that may strongly suggest the deposition of CPPD crystals and mitigate against the other diagnoses. Chief among these findings are the presence of chondrocalcinosis (calcification of joint cartilage). This may occur in either fibrocartilage or hyaline cartilage.
The precise mechanism for the occurrence of CPPD is uncertain. It has been postulated that the increased breakdown of adenosine triphosphate (ATP) results in greater amounts of inorganic pyrophosphate, which may change the cartilage matrix and influence the promotion of CPPD deposition (1).

This breakdown may be influenced by age and genetic makeup. Exuberant activity of the enzymes that metabolize triphosphates has been noted in CPPD patients. The inorganic phosphates are capable of binding to calcium and precipitate crystal deposition in cartilage and joint synovium.
Calcification of the hyaline and fibrocartilage may occur as well as synovial membrane calcification. The major joints involved in descending order of frequency are as follows; knee, wrist, hand, hip, shoulder, elbow, foot, pelvis and spine (2).
In the knee, meniscal calcifications may assume a triangular configuration on the AP view; however, these may also be seen on the lateral view. Figure 1 demonstrates this meniscal calcification, most prominently at the margins of the joint, but also as a thin line of calcification that extends through the joint spaces. Calcification of the hyaline cartilage of the femoral condyles can present as a fine line of calcification paralleling the articular surfaces. Chondrocalcinosis may precede the appearance of the usual findings of joint degeneration, i.e., joint thinning and osteophyte formation. Because a small percentage of patients over the age of 60 years may have chondrocalcinosis without CPPD, preferential degenerative involvement of the patellofemoral compartment without apparent medial compartment involvement may be characteristic of CPPD and help to differentiate it from DJD. The presence of subchondral sclerosis and prominent subchondral cyst formation is common.
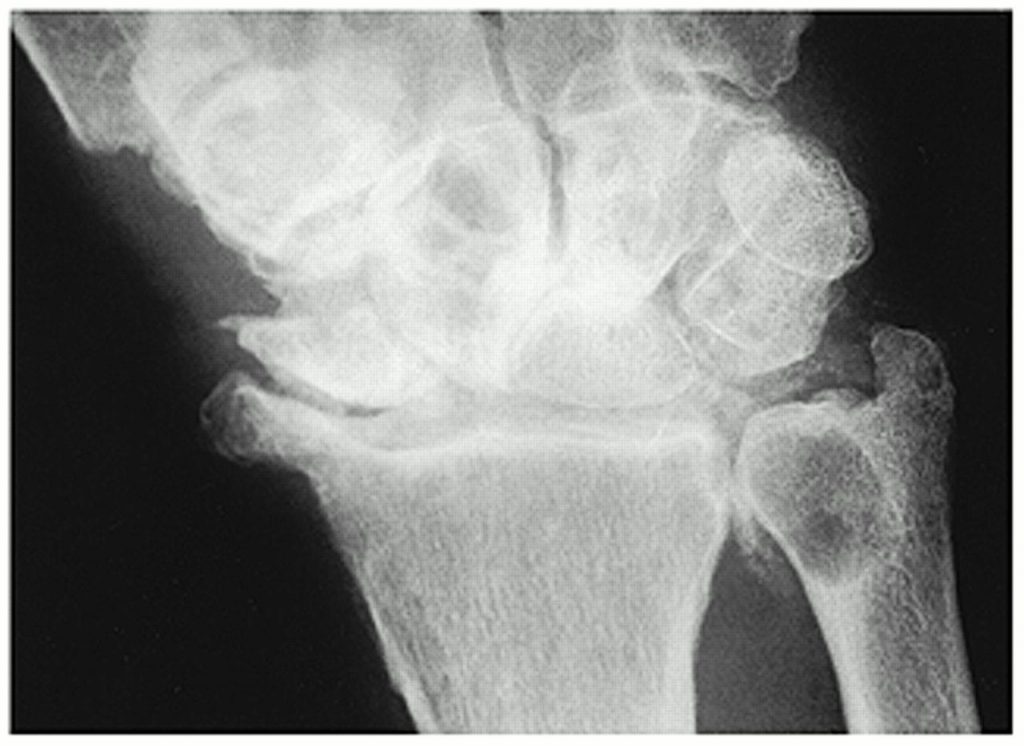
Wrist involvement typically features changes consisting of joint thinning at the radiocarpal articulation, specifically at the radioscaphoid articulation, with subchondral sclerosis and cyst formation. Chondrocalcinosis takes the form of calcification of the triangular fibrocartilage at the ulnar aspect of the joint and hyaline cartilage calcification at any of the carpal bones. There may be disruption of the scapholunate ligament and subsequent widening of the scapholunate interval. Accompanying rotation abnormalities of the scaphoid and lunate may allow the capitate to migrate proximally. This constellation of findings is termed a “scapholunate advanced collapse (SLAC) deformity.” Figure 2 demonstrates a hazy chondrocalcinosis in the triangular fibrocartilage with a SLAC deformity and a large subchondral cyst in the distal ulna. There is marked thinning of the radiocarpal joint with marginal joint proliferation.
Spinal manifestations are relatively infrequent. The lumbar spine is involved more often than the cervical spine. Radiographically it may simulate the syndesmophyte formation of ankylosing spondylitis. This is the result of thin, vertical calcification of the outer fibers of the anulus fibrosis. Other changes are relatively non-specific and include loss of vertebral body height, vacuum phenomenon, osteophyte formation, endplate sclerosis, and facet arthrosis. These manifestations are demonstrated in figure 3.

In conclusion, evaluate the articular cartilage whenever you see other findings of degeneration. If there is chondrocalcinosis, CPPD is the most likely diagnosis.
References:
- Saadeh C., Diamond H.: “Calcium Pyrophosphate Deposition Disease”; Medscape, July 15, 2016.
- Yochum T.R., Rowe L. J.: Essentials of Skeletal Radiology, ed 3. Philadelphia, Lippincott Williams & Wilkins, 2005.



















