Spinal Schwannomas
Spinal schwannomas represent nerve sheathe tumors and arise from Schwann cells. Schwann cells produce myelin, which is the layer comprising the nerve sheathe. Small spinal Schwannomas often produce no symptoms. Symptoms, when present, may consist of intermittent pain in the nerve distribution. The following case study is of a patient in whom cervical radiculopathy initially prompted a presumptive diagnosis of disc herniation and warranted performing an MRI examination.
A 59-year-old male presented to his doctor for a complaint of left upper extremity numbness. Orthopedic testing did not yield specific results for a cervical disc herniation, and routine cervical x-ray study reported only minor degenerative changes. A presumptive diagnosis of a herniated cervical disc was made. The patient was placed on a trial program of manipulation. A limited degree of improvement was noted after several weeks. The patient discontinued care on his own, but returned several months later with the same complaint. Manipulation was again provided with similar results. There was limited improvement; however, the condition did not resolve. After nearly a year, the patient returned a third time with a slightly worsened complaint of left upper extremity numbness. It was decided at the time to obtain an MRI examination of the cervical spine to attempt to better ascertain the source of the patient’s symptoms.
The decision to order the MRI was based on two factors:
- Failure of adequate response to conservative treatment; and
- Presence of worsening neurologic symptoms.
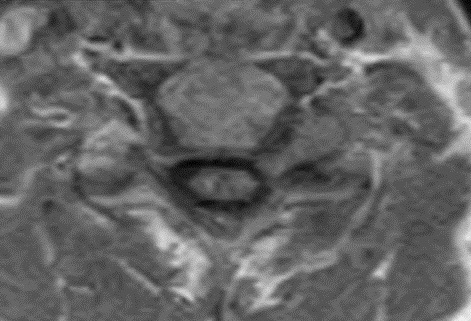
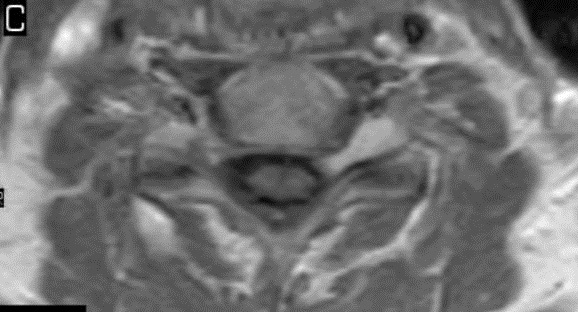
I have provided some select images from the MRI study that was obtained. Initially, the study was ordered non-contrast. Fig. 1 is a midline T-2 weighted image. It demonstrates a degree of posterior disc bulging at C6-C7. No focal posterior discal prominence was noted that would indicate a herniation. Fig. 2 is a gradient echo weighted image through the C6-C7 disc space. In this image, there is obvious expansion of the left intervertebral foramen with a degree of erosion of the facet at the posterior margin of the foramen. The signal intensity is bright on this image, compared to the normal intermediate signal intensity noted within the right foramen. You will note a degree of irregularity at the posterior margin of the disc in this cut, consistent with the disc bulging seen on the sagittal images. There is not sufficient encroachment of the central canal however to account for a neurologic deficit. A left parasagittal STIR image (Fig.3) reveals an obvious focus of abnormal signal within the left C6-C7 IVF that corresponds to the finding that was noted on the axial image. The signal intensity of this area was high on the STIR, gradient echo, and T-2 weighted images, and low on the T1 weighted images, consistent with fluid. At this point what diagnoses would you entertain, and would you order any follow-up imaging or testing?


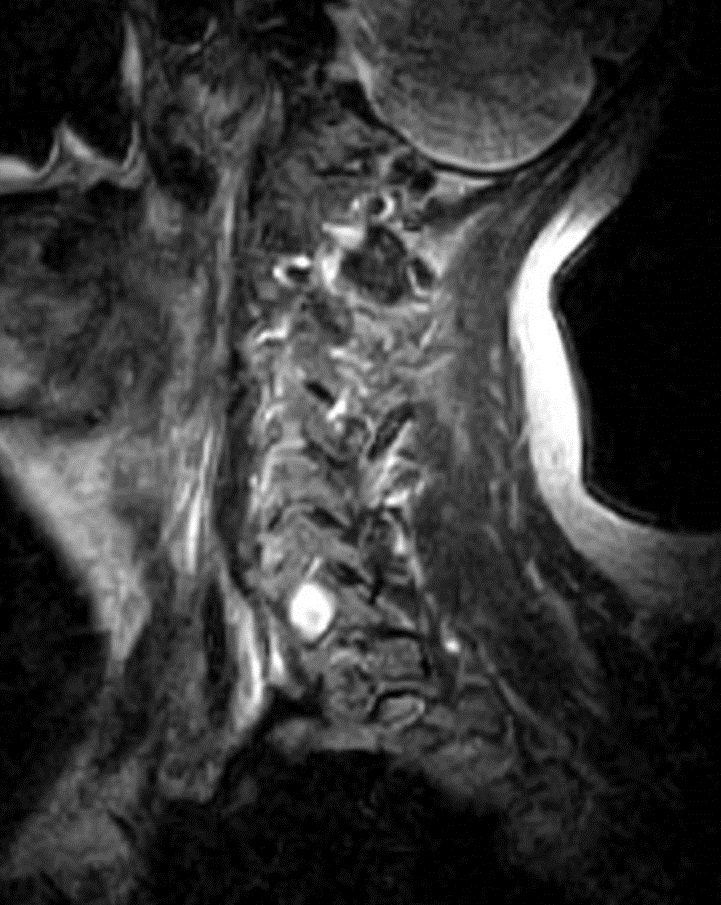
The fluid characteristics of this lesion may be consistent with two probable considerations. It is possible that there is dilation of the dural root sleeve and that the signal represents cerebrospinal fluid. This condition is not neoplastic, but rather developmental, and does not constitute a major health concern. Another possibility is that the lesion does represent a neoplastic process. Both conditions may look similar on MRI. A rather simple way to distinguish between the two would be to perform a follow-up MRI examination with the administration of intravenous contrast (gadolinium). If the mass is neoplastic there would be expected enhancement of the mass, the signal would become brighter on the T-1 weighted postcontrast images. If the mass simply represents a fluid filled sac, such as dural root sleeve dilation or cyst, there will be no enhancement of the mass.
This patient underwent a second limited contrast examination. Pre- and post-contrast T-1 weighted images were obtained. Fig. 4 represents the pre-contrast T-1 weighted image, and Fig. 5 represents the post-contrast image at the same level. There is a quite definite increase in signal intensity of the mass on the post-contrast images. Thus, the mass is said to enhance and this is indicative of a neoplastic process. The most common extradural intraforaminal mass is a schwannoma, which represents a nerve sheathe tumor. This was the presumptive diagnosis as the patient underwent surgery for removal of the tumor. Subsequent biopsy of the lesion confirmed schwannoma. The patient did well post- surgery and the left upper extremity symptoms resolved.
Schwannomas are differentiated as type 1, type 2, type 3, and type 4.
-Type 1 tumors are found within the dura and represent the most common type.
-Type 2 tumors start as a type 1 but continue to grow through the IVF and thus have a second component outside the spine.
-Type 3 tumors start outside the spinal canal and represent paraspinal nerve sheath tumors.-Type 4 begin as a type 3 and grow through the IVF into the spinal canal.
MRI examinations can allow the visualization of lesions as small as a few millimeters. Schwannomas have been associated with the conditions neuraobibromatosis II (NF2) and schwannomatosis. If either of these two conditions is not present, the lesion is said to be a sporadic schwannoma. Schwannoma represents the most common type of nerve sheathe tumor. The most common nerve sheathe tumor in the thoracic spine is the schwannoma (1). They usually seen in the 4th decade of life when occurring sporadically.
Treatment may include microsurgery (2), as was performed in this case. Small lesions without symptoms may be followed with periodic MRI scans.
Schwannomas may be a diagnostic consideration in cases with radiculopathy that do not clinically fit the classic disc herniation picture.
References
- Renfrew D.L.: Atlas of Spine Imaging, Philadelphia, Saunders, 2003
- Yochum T.R., Rowe L.J.: Essentials of Skeletal Radiology, ed 3. Philadelphia, Lippincott Williams & Wilkins, 2005.