Knee Pain

Patellofemoral pain syndrome (PFPS), also called “Runner’s Knee,”, describes the symptom complex of knee discomfort, swelling or crepitus that results from excessive or imbalanced forces acting on the joint. PFPS can be traumatically induced but more commonly results from muscular imbalance and cumulative overload. It is the most common cause of knee pain in the general population, affecting an estimated 25% of adults. (1,5,23) Many PFPS patients are young and athletic. (32) Data suggests the condition may affect nearly 10% of young athletes. (2)
Normal patellar tracking is dependent upon the static and dynamic stabilizers of the patella acting in concert. Imbalances in these stabilizers can alter the distribution of forces to the patellofemoral articular surfaces and related soft tissues. Researchers estimate that patellofemoral forces are between 1/3 and 1/2 of a person’s body weight while walking and can increase almost 20 fold when squatting. (3) Biomechanical tracking stresses are quickly compounded, causing irritation to the patellofemoral cartilage and eventual patellofemoral degeneration.
PFPS
PFPS is most commonly related to lateral tracking of the patella. (4) The patella has a natural tendency to migrate laterally due to the pull of the quadriceps and the slight natural valgus of the lower extremity. (5) Compounding this problem it the fact that the patellofemoral orientation is largely determined by the hip and foot. (6,7) Pes planus causes internal rotation of the tibial and subsequent deviation of the patella-increasing one’s risk of PFPS. (8,24) Gluteus medius weakness results in valgocity of the knee and subsequent lateral tracking. Current research suggests that patellar movement and tracking is more dependent on global femur and tibia biomechanics than any individual knee muscle strength. (26)
Additional risk factors for the development of PFPS include joint overload/ overuse; trauma; tight lateral knee capsule; patellar hypermobility; and muscular imbalance, particularly quadriceps or iliotibial band hypertonicity and vastus medialis or quadriceps weakness. (9,28-30)
Symptoms
PFPS patients generally present with dull peripatellar pain that is exacerbated by activities that load the joint, including prolonged walking, running, squatting, jumping, kneeling, arising from a seated position or stair climbing, especially walking down stairs or downhill. Swelling may accompany the pain. Disruption of patellofemoral cartilage may result in crepitus, intermittent locking or giving way. (27)
Testing and Diagnosis
Clinical evaluation of PFPS should be directed toward identifying factors that create an imbalanced force on the patella. PFPS patients often have hypertonic soleus, hamstring, iliopsoas, piriformis, and thigh adductor muscles with tightness in the iliotibial band and posterior hip capsule. (8,9,10) Weakness in the quadriceps or hamstring muscles increases one’s risk of developing the problem three to five fold. (24) Weakness in the gluteus maximus or medius is common in patients with knee pain and contributes to PFPS. (12,33) Gluteus medius weakness may be assessed by observing for pelvic drop or knee valgus (Trendelenberg sign) when performing a single leg stand, overhead squat test, single leg squat, or single leg 6” step down.
Palpation generally reveals peripatellar tenderness with exacerbation of symptoms upon patellar compression. Clinicians may consider alternatives to the Patellar grind test (aka Clarke sign), as this assessment has been shown to be unreliable and may even generate new complaints. (34,35) Patellar mobility may be assessed with the Patellar Glide test and Patellar tilt test, or by observing patellar tracking during active knee flexion/ extension (Patellar tracking assessment). (36) A static assessment of patellofemoral orientation is an unreliable measurement tool. (13,14) Historically, increased Q angles were thought to increase lateral pressures and were considered an etiologic factor. (31) Newer studies show that normal Q angles vary from 10 to 20 degrees and are similar in symptomatic and non-symptomatic patellofemoral patients. (15,16)
Differentiation of meniscal pain from patellofemoral pain may be accomplished by having the patient perform a two-legged squat. Meniscal pain is expected at the bottom of the squat, while patellofemoral pain is present during descent and ascent.
Imaging
Knee radiographs may be necessary to rule out fractures in those with a history of trauma or osteoarthritis and in patients older than 50. Radiographs may also be appropriate in patients with significant swelling, a recent history of knee surgery and in those whose pain does not improve with a trial of treatment. (17) The radiographic assessment of PFPS would include a standing lateral, AP, sunrise, and patellofemoral (merchant) view.
The differential diagnosis for anterior knee pain includes fracture, infection, neoplasm, patellar or quadriceps tendinopathy, Osgood-Schlatters disease, bursitis and cartilaginous irritation including osteochondritis dissecans, chondromalacia patella, and patellofemoral arthritis. Additional considerations would include Sinding-Larsen-Johansson syndrome, plica, iliotibial band syndrome, symptomatic bipartite patella and referred pain from the spine or hip. (18)
Treatment
Management of PFPS should progress from the minimization of aggravating factors and anti-inflammatory measures to the long-term correction of functional deficits. Decreasing fear-avoidance behavior may lead to improved outcomes. (30) Lifestyle modification may be necessary to reduce pain-provoking activities, especially running, jumping and activities that induce valgus stress. Athletes should avoid allowing their knee to cross in front of their toes while squatting. Electrotherapy and ice may be useful initially for the reduction of pain and inflammation. Russian Stim (10:30) is a consideration to activate the VMO. NSAIDS or anti-inflammatory medication may provide short-term benefits for the relief of pain and inflammation.
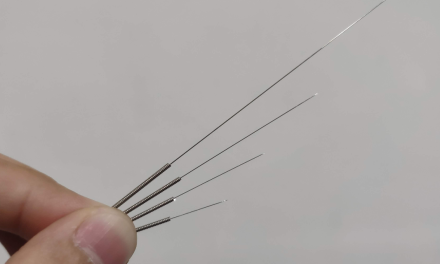
Myofascial release and stretching should be directed at hypertonic muscles, including the TFL, gastroc, soleus, hamstring, piriformis, hip rotators, and psoas. Myofascial release or IASTM may be appropriate for tightness in the iliotibial band, vastus lateralis, posterior hip capsule and lateral knee retinaculum.
Since gluteus medius and VMO weakness are key factors in the development of PFPS and knee pain, strengthening exercises are generally necessary for those muscles. (19) Stabilization exercises may include pillow push (push the back of your knee into a pillow for 5-6 seconds), supine heel slide, terminal knee (short-arc) extension, clam, glut bridge, semi-stiff deadlift, posterior lunge and monster walk. Eccentric quadriceps strengthening is more effective than concentric exercise in the treatment of PFPS. (25)
Conclusion
Manipulation may be necessary for restrictions in the lumbosacral and lower extremity joints. Hypermobility is common in the ipsilateral SI joint with restrictions present contralaterally. Patellofemoral problems are part of a complex biomechanical chain and corrective taping, including “McConnell taping” is generally ineffective. (20,21) Kinesiotape for PFPS has anecdotal support.
Arch supports or custom orthotics may be necessary to correct hyperpronation. Research has shown that runners with PFPS benefit from a combination of exercise and foot orthotics. (22) Runners should change shoes every 250 to 500 miles. Sequelae of unmanaged PFPS include accelerated degenerative changes and sedentarism. A surgical “lateral release” of the lateral retinaculum is the last resort when conservative measures have failed.
References
1. Baquie P, Brukner P. Injuries presenting to an Australian sports medicine centre: a 12-month study. Clin J Sport Med. 1997;7:28-31.
2. Myer GD, Ford KR, Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010; 25:700–7.
3. Reilly DT, Martens M. Experimental analysis of the quadriceps muscle force and patellofemoral joint reaction force for various activities. Acta Orthop Scand. 1972;43:126–37.
4. Doucette SA, Goble EM. The effect of exercise on patellar tracking in lateral patellar compression syndrome. Am J Sports Med. 1992;20:434-440.
5. Wilson T, The Measurement of Patellar Alignment in Patellofemoral Pain Syndrome: Are We Confusing Assumptions With Evidence? JOSPT June 2007, Vol 37, Number 6
6. Griffin LY, Agel J, Alborhm MJ, et al. Non-contact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg, 2000;8:141-50
7. Bobbert MF, van Zandwijk JP. Dynamics of force and muscle stimulation in human vertical jumping. Med Sci Sports Exerc, 1999;31:303-10
8. Zappala FG, Taffel CB, Scuderi GR. Rehabilitation of patellofemoral joint disorders. Orthop Clin North Am. 1992;23:555–66.
9. Puniello MS. Iliotibial band tightness and medial patellar glide in patients with patellofemoral dysfunction. J Orthop Sports Phys Ther. 1993;17:144–8.
10. Liebenson C. Functional problems associated with the knee—Part one: Sources of biomechanical overload Journal of Bodywork and Movement Therapies (2006) 10, 306–311
12. Ireland ML, Willson JD, Ballantyne BT, McClay-Davis I. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther, 2004;33:671-6.
13. Fitzgerald GK, McClure PW. Reliability of measurements obtained with four tests for patellofemoral alignment. Phys Ther. 1995;75:84-92
14. Watson CJ, Propps M, Galt W, Redding A, Dobbs D. Reliability of McConnell’s classification of patellar orientation in symptomatic and asymptomatic subjects. J Orthop Sports Phys Ther. 1999;29:378-385; discussion 386-393
15. Tomsich DA, Nitz AJ, Threlkeld AJ, Shapiro R. Patellofemoral alignment: reliability. J Orthop Sports Phys Ther. 1996;23:200–8.
16. Reid DC. Sports injury assessment and rehabilitation. New York: Churchill Livingstone, 1992:345–98.
17. Dixit S, Difiori JP. Management of Patellofemoral Pain Syndrome. Am Fam Physician. 2007 Jan 15;75(2):194-202.
18. Calmbach WL, Hutchens M. Evaluation of patients presenting with knee pain: Part II. Differential diagnosis Am Family Phys 2003. Sept 1;68(5) 917-922
19. Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther, 2003;33:639-46
20. Warden S J, Hinman RS, Watson MA Jr, et al. Patellar taping and bracing for the treatment of chronic knee pain: a systematic review and meta-analysis. Arthritis Rheum 2008; 59:73–83.
21. McConnell JS. The management of chondromalacia patellae: a long-term solution. Aust J Physiotherapy. 1986;32:215–23.
22. Eng JJ, Pierrynowski MR. Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome. Phys Ther 1993; 73:62–8; discussion 68–70
23. Tobin S, Robinson G. The effect of McConnell’s vastus lateralis inhibition taping technique on vastus lateralis and vastus medialis obliquus activity. Physiotherapy. 2000;86:173-183.
24. Boling MC, Padua DA, Marshall SW, et al. A Prospective Investigation of Biomechanical Risk Factors for Patellofemoral Pain Syndrome. Am J Sports Med November 2009 vol. 37 no. 11 2108-2116
25. Ashraf Ramadan Hafez, Abdulrahim Zakaria and Syamala Buragadda, Eccentric versus Concentric Contraction of Quadriceps Muscles in Treatment of Chondromalacia Patellae World Journal of Medical Sciences 7 (3): 197-203, 2012
26. Sawatsky A et. al, Changes in patellofemoral joint contact pressures caused by vastus medialis muscle weakness Clinical Biomechanics 27 (2012) 595–601
27. Thomee R, Augustsson J, Karlsson J. Patellofemoral pain syndrome: a review of current issues. Sports Med 1999;28:245-62.
28. Waryasz GR, McDermott AY. Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dynamic Medicine. 2008, 7:9. doi:10.1186/1476-5918-7-9.
29. Lankhorst NE, Bierma-Zeinstra SMA, Middelkoop MV. Risk Factors for Patellofemoral Pain Syndrome: A Systematic Review. J Orthop Sports Phys Ther. Epub 25 October 2011. Doi: 10.2519/jospt 2012.3803.
30. Piva SR, Fitzgerald GK, Wisniewski S, Delitto A. Predictors of pain and function outcome after rehabilitation in patients with patellofemoral pain syndrome. J Rehabil Med. 2009; 41(8): 604–612. doi: 10.2340/16501977-0372.
31. Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. Jun 1984;66(5):715-24.
32. Dixit S, Burton M, Mines B. Management of Patellofemoral Pain Syndrome. Am Fam Physician. 2007 Jan 15;75(2):194-202.
33. Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip Strength and Hip and Knee Kinematics During Stair Descent in Females With and Without Patellofemoral Pain Syndrome. J Orthop Sports Phys Ther. 2008;38(1):12-18. doi:10.2519/jospt.2008.2462.
34. Abernethy P, Wilson G, Logan P. Strength, and power assessment. Issues, controversies, and challenges. Sports Med 1995;19:401-17.
35. Scott T Doberstein, MS, LAT, ATC, CSCS, Richard L Romeyn, MD, and David M Reineke, Ph.D. The Diagnostic Value of the Clarke Sign in Assessing Chondromalacia Patella J Athl Train. 2008 Mar-Apr; 43(2): 190–196.
36. Cook C, Mabry L, Reiman M, Hegedus E. Best tests/clinical findings for screening and diagnosis of patellofemoral pain syndrome: a systematic review Physiother. 2011,