Dry Needling Coding and Reimbursement for Chiropractic
While the clinical concept behind dry needling is relatively straightforward, the reimbursement, coding, and coverage rules are anything but. Missteps can lead to denied claims, compliance concerns, or uncomfortable patient conversations about coverage and cost.
Background
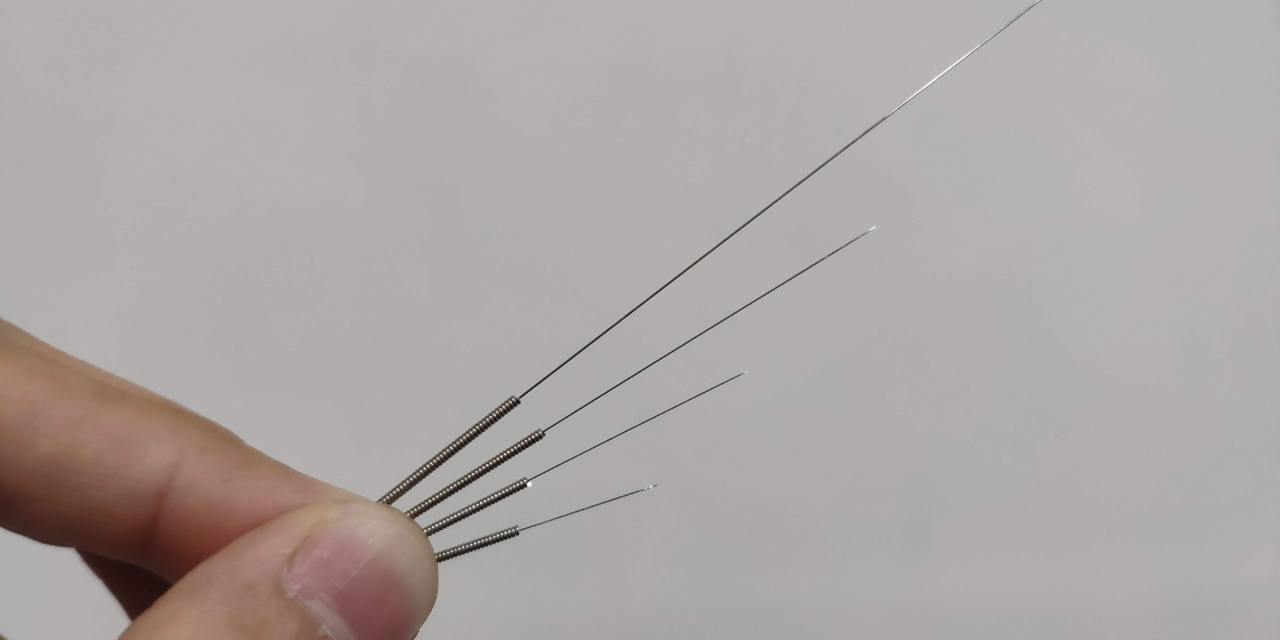
Dry needling differs from acupuncture in its origin (Western versus Eastern medicine), target (trigger points versus meridians), and scope (musculoskeletal system versus whole body). It is a way to target myofascial trigger points by inserting a thin needle (that does not contain any medication, hence “dry”) into the muscles to relieve pain and speed up healing by increasing blood flow to the affected area. The muscles usually contract or twitch, which indicates that the treatment is working. It is typically used as an adjunctive procedure along with other musculoskeletal treatments for pain.
Trigger points are created when overused muscle fibers don’t get enough oxygen and nutrients as the blood flow is limited. As a result, the tissue in that area becomes acidic, and the nerves become more sensitive, which leads to local or even referred pain. Dry needling can stimulate the area to restore blood flow to release tension, and flush out the area. It may also stimulate endorphin release, which is the body’s natural painkiller.
Diagnosis Coding
“Trigger points” is not found in the alphabetic index of ICD-10-CM, which is where we find the diagnosis codes used to report the rationale for treatment that is billed to third parties via the CMS-1500 claim form. However, M79.1-, the subcategory for codes for myalgia, has an inclusion term “myofascial pain syndrome.” This is generally accepted as synonymous with trigger points, but documentation would be stronger if the phrase in the record matches the code description. The diagnosis code options include:
- M79.10 Myalgia, unspecified site
- M79.11 Myalgia of mastication muscle
- M79.12 Myalgia of auxiliary muscles, head and neck
- M79.18 Myalgia, other site
Given the options for describing anatomic location, the most common code chiropractors might report would be M79.18, which covers everywhere other than mastication muscles and auxiliary muscles of the head and neck.
Other diagnoses that might be worth considering include:
- M60.8- Other myositis (with the fourth and fifth characters identifying the anatomic location)
- M79.7 Fibromyalgia
- G44.2- Tension-type headache (with the fourth and fifth characters providing more detail about the chronicity and intractability of the headache)
- M54- Dorsalgia (with the fourth and fifth characters providing details about the location of the pain)
- M46.0- Enthesopathy (with the fourth character detailing the anatomic location)
Note that each of these conditions has its own diagnostic criteria, which should be clearly documented in the record. (The “-“ after some of these codes indicates that they are not complete here, and users should look up the additional characters in order to select the most accurate code.)
Procedure Coding
Two Current Procedural Terminology codes (CPT, copyright 2025 American Medical Association) exist for dry needling:
- 20560 Needle insertion(s) without injection(s); 1 or 2 muscle(s)
- 20561 Needle insertion(s) without injection(s); 3 or more muscles
Based on these code descriptions, the specific muscles should be clearly documented, to establish if 3 or more were treated. These are relatively new codes, having been added to the CPT code book in 2020. They were added because this type of work is not synonymous with the existing codes for traditional acupuncture or an injection procedure. Prior to the new codes, dry needling was sometimes reported with 97140 Manual therapy techniques, because it is used to report manual trigger point work, but this code was not a good fit for non-manual procedures. As of 2020, the parenthetical note for 97140 directs users to code 20560 or 20561, and payers typically would not allow the use of 97140 for dry needling.
At the time of this writing, the nationally unadjusted relative value unit (RVU) for 20560 is 0.760 and for 20561 is 1.110. For comparison, this is relatively close to the RVU for the familiar chiropractic manipulative treatment (CMT) codes 98940 and 98941. This means that, when determining dry needling fees, it would be defensible if they were similar in value to the CMT codes, based on the standard and generally accepted RVU rationale.
If a payer does cover this service, the GP modifier might be required. This informs the payer that the services were delivered under an outpatient physical therapy plan of care. Check with the payer to be sure. These codes do not appear to have any bundling issues with other common chiropractic CPT codes; however, they cannot be billed along with acupuncture (97810-97814) at the same encounter. No additional modifier (such as 59 distinct procedural service, or XS separate structure) will bypass this edit.
Coverage
The scope of practice for chiropractic physicians in Illinois includes dry needling. However, providers should seek sufficient training to ensure that the standard of care has been met and that patients are safe.
Dry needling may be helpful to treat conditions like back and neck pain, headaches, TMJ disorders, carpal tunnel, night cramps, and more. However, Medicare only covers dry needling (along with acupuncture) for chronic low back pain, meaning the condition has lasted at least 12 weeks and isn’t tied to a known cause, such as an infection. Yet, providers must be a doctor (or nurse practitioner or physician’s assistant) with a master’s or doctoral level degree in acupuncture or Oriental Medicine from an accredited institution. Therefore, many chiropractors will not be eligible to deliver dry needling for Medicare reimbursement.
Most private payers, like Blue Cross Blue Shield of Illinois (see Policy Number SUR702.018) consider dry needling to be “experimental, investigational, and/or unproven.” They cite the fact that manual identification of trigger points has not been established to be reliable and that the physiologic basis for the treatment is not well described in the literature. As such, when it comes to insurance coverage, dry needling is often not included, but providers should always verify benefits and/or review the patient’s summary plan description.
When providing non-covered services, providers should notify patients, in writing, ahead of time. A Good Faith Estimate (GFE) is a compliant way to do this. If a discount is offered, consider using a state-registered Discount Medical Plan Organization, like ChiroHealthUSA, to avoid the appearance of a dual fee schedule.
Conclusion
When done properly, dry needling can be a powerful adjunctive therapy to other treatments available in a chiropractic office. Once providers understand the coding, documentation, and coverage issues, this service may be beneficial to the practice and to patients alike.