
Atypical Proximal Femoral Fracture: An Important Diagnostic Consideration for Patients With Hip, Groin, Or Thigh Pain
[Editor’s note: Dr. Ruof is presenting the webinar “Pathologic Insufficiency, and Stress Fractures – How Can I Diagnose and Differentiate?” on Tuesday January 30, 2024. Register for the webinar here.]
Hip pain is a common complaint of many chiropractic patients, particularly those patients that are older and may be suffering from arthritis. Additionally, the risk of femoral neck fractures in people, particularly women, with osteoporosis is well understood by clinicians and patients alike. In an osteoporotic patient with hip pain, one of the first etiologies that must be ruled out is a femoral neck fracture. However, there is another less common, and less well-understood, condition that may result in hip pain in the osteoporotic patient.
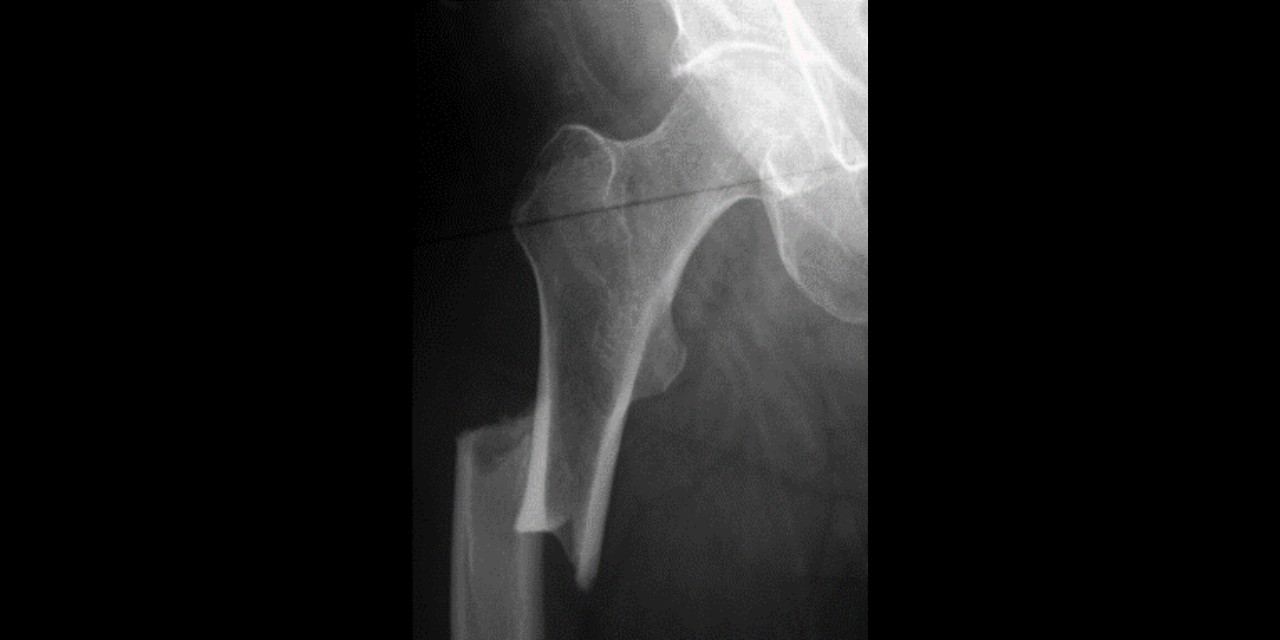
Our patient is a 65-year-old female with groin pain for three months. The pain is dull and unrelenting without an inciting traumatic event. Orthopedic tests were non-specific and an AP radiograph of the hip was performed. Figure 1 demonstrates a focal periosteal reaction with cortical thickening along the lateral cortex of the proximal femoral diaphysis. A horizontal radiolucent fracture line is visualized traversing this area of cortical thickening. This finding demonstrates an incomplete insufficiency fracture of the proximal femoral diaphysis, known as an atypical fracture of the proximal femur.

An increased risk in this type of fracture is seen in patients that are on long-term bisphosphonate therapy (greater than 3-5 years). Bisphosphonates are currently the most popular medication to treat osteoclast-mediated bone resorption diseases. This most commonly includes osteoporosis, but other conditions include Paget’s disease and metastatic bone disease. Commonly prescribed bisphosphonates include Actonel, Fosamax, Boniva, Reclast, and Aredia.
The clinical presentation of an atypical proximal femoral fracture includes groin, hip, or thigh pain of weeks to months duration. A fracture can be completely atraumatic or result from a low-energy injury such as tripping on a stair or falling from standing. These fractures are often bilateral but may be in asynchronous degrees of fracture formation. The risk of this fracture is extremely low in untreated women over 55 years old, with a rate of 0.02 per 1000 women. This risk increases to 1 in 1000 in older women treated with long-term bisphosphonate use.
The proposed theory regarding histologic cause of this type of fracture is that prolonged bisphosphonate use decreases osteoclast activity and inhibits bone remodeling. This inhibition leads to chronic microdamage that would be repaired under normal circumstances, but repair is inhibited and leads to increased skeletal fragility.
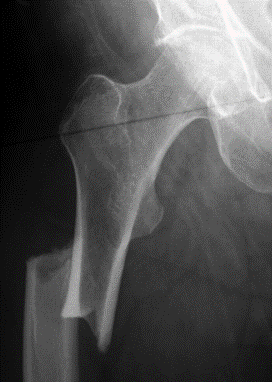
It is important to understand the radiographic findings of an early incomplete atypical proximal femoral fracture, as the radiographic findings can be extremely subtle. In some cases, the only finding is focal cortical thickening (figure 2). This fracture always starts at the lateral cortex and will progress medially. It is found distal to the subtrochanteric region within the diaphysis. The fracture is usually transverse or oblique and may have a “beaked” appearance of one cortex (figure 3).

Another important clinical feature of this fracture pattern is that it is often bilateral. Because long-term bisphosphonate use results in systemic inhibition of osteoclastic activity, both proximal femora are undergoing the same increase in skeletal fragility, and, therefore, an increase in bilateral fractures is important to assess clinically. If an incomplete fracture is found, imaging of the contralateral side is imperative, even in the absence of contralateral symptoms. A long-bone radiograph of the femur should be performed, as this fracture can be found quite distally in the femur. If the radiographs are negative but clinical suspicion or unilateral fracture is found, MR imaging of the femur (not the hip) should be performed.
Once an atypical femoral fracture has been diagnosed, it is advised that bisphosphonate therapy be discontinued. Most fractures, even incomplete, are treated with surgical fixation (intramedullary nail reconstruction). Conservative treatment may be considered in patients in which weight-bearing can be effectively limited, but surgical fixation is typically performed if there is no symptomatic or radiologic improvement after 2-3 months. Prophylactic operative treatment is even often performed in patients with pain and focal cortical thickening to prevent progression to complete fracture.
While this is an uncommon fracture, it should be considered in patients undergoing long-term bisphosphonate use accompanied by hip, thigh, or groin pain. This article does not suggest that patients receiving bisphosphonate therapy should discontinue its use; research reveals that the risk of osteoporotic-related vertebral body or proximal femoral neck fractures are greater in high-risk osteoporotic patients that are untreated. The goal is make clinicians aware of this uncommon type of fracture in a population that we, as chiropractic physicians, treat on a regular basis. Proper imaging can help decrease the risk of an incomplete fracture progressing to a complete fracture, greatly improving the prognosis of the affected patient.
References
Isaacs JD, Shidiak L, Harris IA, Szomor ZL. Femoral insufficiency fractures associated with prolonged bisphosphonate therapy. Clin Orthop Relat Res. 2010 Dec;468(12):3384-92.
Silverman S, Kupperman E, Bukata S. Bisphosphonate-related atypical femoral fracture: Managing a rare but serious complication. Cleveland Clinic Journal of Medicine November 2018, 85 (11) 885-893.
Porrino JA, Kohl CA, Taljanovic M et-al. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol. 2010;194 (4): 1061-4.
Yoon RS, Hwang JS, Beebe KS. Long-term bisphosphonate usage and subtrochanteric insufficiency fractures: a cause for concern? J Bone Joint Surg Br. 2011 Oct;93(10):1289-95.



















