
Upper vs. Lower Motor Neuron Lesions

A quick review of the anatomy, signs, and symptoms of what we may see in practice is a great way to keep our minds sharp and patients safe. I recently had the pleasure of examining a patient who had presented with lower right sided radicular pain and weakness. After a thorough history, I discovered that she also was experiencing ipsilateral upper extremity weakness in the absence of pain. Further examination revealed that her weakness did not follow a nerve root pattern, and she had a positive Babinski sign. Needless to say, I was very excited and could not resist testing it over again. It is so rare that we get the opportunity to actually see first hand the signs we learned about in school without having to see them on YouTube.
Motor Neuron Lesion
An upper motor neuron lesion is a lesion of the neural pathway above the anterior horn of the spinal cord or motor nuclei of the cranial nerves. A Lower motor neuron lesion is a lesion which affects nerve fibers traveling from the anterior horn of the spinal cord to the associated muscle(s).1
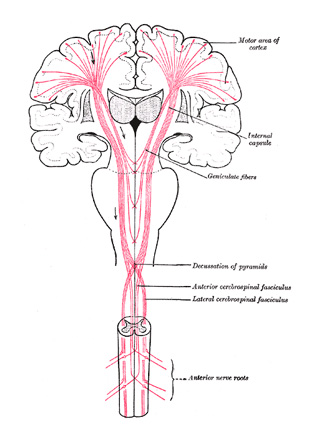
When the spinal cord develops, the posterior part becomes responsible for managing most aspects of sensation, and the anterior is more responsible for movement. When you move, the cells of your cerebral cortex send a message to cells in the spinal cord. These cells then relay the message out to the peripheral nervous system and muscles. The nerve cells that are responsible for relaying messages between the brain and the peripheral nervous system are called motor neurons. The nerves that send messages between the cerebral cortex and the spine are called upper motor neurons, and those that relay messages from the spine to the muscles are called lower motor neurons.
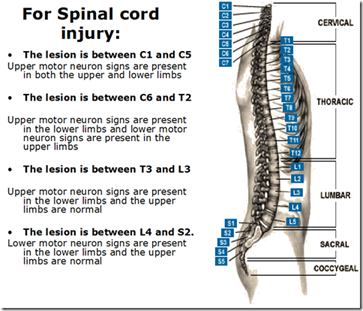
When we think of upper motor neuron lesions we think tumors, stroke, ALS, and polio. In this day and age, we are not likely to have a patient with one of these problems walk into our office first. However, an upper motor neuron lesion can also occur as a result of cervical spine injury. In this case, there is a likelihood that this patient may walk into our office; and if this was the case, we probably would not want to miss the diagnosis?
Causes
Some of the likely causes of lower motor neuron lesions are motor neuron disease, peripheral neuropathy, poliomyelitis, and spinal cord injury with nerve root compression. Lower motor neurons control movement in the arms, legs, chest, face, throat, and tongue. Mixed upper and lower motor neuron diseases include multiple sclerosis.
Upper motor neuron lesion signs:
- Weakness – the extensors are weaker than the flexors in the arms, but the reverse is true in the legs
- Muscle wasting is absent or slight
- Hyperreflexia with clonus
- Spasticity
- No fasciculation’s
- Babinski sign positive – extended hallux and flaring of remaining digits
- Hoffmann’s sign is positive if flexion and sudden release of the terminal phalanx of the middle finger result in reflex flexion of all the digits. This is a sign of the presence of reflex activity. It is positive in, but not specific to, upper motor neuron lesions.
- Pronator drift – Patient is asked to hold fully extended arms straight out in front with palms facing upward. If a lesion is present when the patient is asked to close his/her eyes the arm on the affected side pronates due to the difference in muscular tone between pronators and supinators.2
Lower Motor Neuron Lesion findings:
- Weakness – limited to focal or root innervated pattern
- Muscle Wasting – prominent in a focal pattern
- Reflexes – absent or reduced in a lower motor neuron lesion
- Fasciculation’s present in the associated muscle group
- Babinski sign absent – downward going digits
Tests to rule out other diseases or to measure muscle involvement:3

EMG/NCV: Used to diagnose disorders of lower motor neurons, as well as disorders of muscles and peripheral nerves. Nerve conduction studies help to differentiate lower motor neuron diseases from peripheral neuropathy and can detect abnormalities in sensory nerves.
Laboratory tests: Blood tests may be ordered to measure levels of the protein creatine kinase; high levels may help diagnose muscle diseases such as muscular dystrophy.
MRI: Images can help diagnose brain and spinal cord tumors, eye disease, inflammation, infection, and vascular irregularities that may lead to stroke.
References 1James D. Fix (1 October 2007). Neuroanatomy0. Lippincott Williams & Wilkins. pp. 120–. ISBN 978-0-7817-7245-7. Retrieved 17 November 2010.
2 www.gpnotebook.co.uk/simplepage.cfm?ID=503709725
3https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Motor-Neuron-Diseases-Fact-Sheet



















