Lumbar Disc Herniation Terminology

One of the most common reasons given for ordering a lumbar spine MRI examination is to rule out disc herniation. MRI is a very efficient tool for this condition. It is helpful, however, to define several terms to ensure a clear understanding of the described elements of the report. In the past, there has been considerable variation in the terms used from one radiologist to the next to describe disc herniations. It was routine to see a disc herniation described as a “disc bulging” by one radiologist and a “disc herniation” by a second. I have found the article in the journal Spine (vol. 26, no. 5, pp E93-E113) to be very helpful in differentiating a true disc herniation from a disk bulge and to clarify the differences in herniation types.
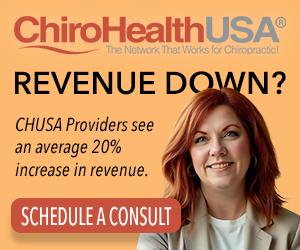
Basically, a “disc bulge” is defined as a prominence of the periphery of the disc that exceeds 50% of the circumference of the disc. A “disc herniation” is defined as a discal prominence that does not exceed 50% of the disc circumference. For comparison purposes, please refer to figure 1. The illustration in the upper left corner demonstrates a diffuse disc bulge. The dotted line represents the margin of the underlying vertebral endplate. The solid outer line represents the margins of the bulging disc. The margins of the disc are increased over 100% of the disc circumference.
A “disc protrusion” is synonymous with disc herniation. Protrusions are classified either as contained, meaning that the outer fibers of the anulus fibrosis are intact of the protrusion, or uncontained, where the fibers are not intact. An uncontained protrusion may also be termed an “extrusion type” herniation. In all cases of protrusion/herniation, the extent of the prominence of the disc does not exceed 50% of the circumference of the disc. The remaining three images in figure 1 represent a broad-based protrusion/herniation, which is contained, a focal protrusion/herniation which is uncontained and an extrusion which is not contained. The last type of disc herniation may also be termed an “uncontained protrusion/herniation.”
The significance of a disc herniation being contained or uncontained may be significant clinically. If the extruded nuclear material extends superiorly of inferiorly away from the parent disc, the herniation is termed “migration.” If the nuclear material loses contact with the parent disc, the herniation is termed “sequestered.”
In image 1, the arrow points to an extrusion type herniation in which the nuclear material maintains contact with the parent disc. In image 2, there is an oval extruded fragment that has lost connection with the disc. This is an example of a sequestered disc.

Image 1 
Image 2
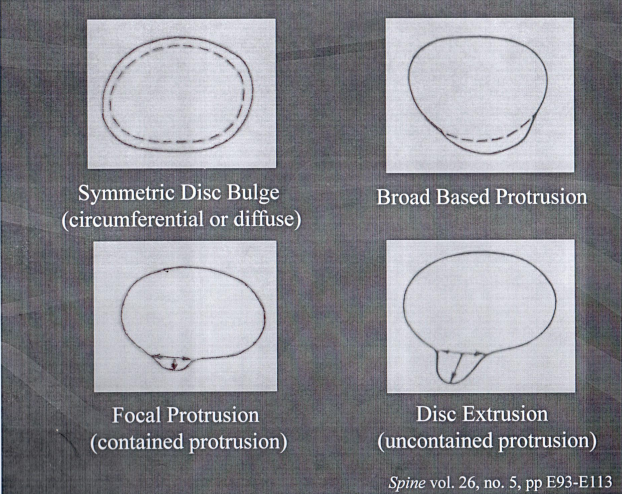
The MRI report must accurately describe the position of a disc herniation. Figure 2 is a representation of an axial cut through a lumbar disc with the vertebral disc outlined at the superior aspect of the image and the posterior arch inferiorly. “C” stands for a central herniation, “PC” for paracentral, “F” for foraminal and “EF” for extraforaminal. Extraforaminal is also sometimes called “far lateral.”
Lumbar disc herniations are also graded according to size. An AP dimension of the disc that measures less than 5.0 mm is small, 5.0-10.0 mm is termed moderate and greater than 10 mm is a large herniation.

The final element in the description of disc herniations is the effect on the thecal sac. If the herniation encroaches upon the central canal of the segment with 50% or greater compromise of the contents, the effect is said to be severe. Encroachment of 25-50% is moderate and 25% or less is minor. If there is compression of a descending nerve root, this needs to be described as well. Image 3 reflects compression of the right descending nerve root. The left root is seen as a hypodense circular shape adjacent to the left facet joint. A white arrowhead points to a right paracentral disc herniation. The normally hypointense nerve root is obliterated by the herniation.
Universal usage of the terms outlined in this article would help to alleviate the confusion that results from the use of inconsistent terminology and would allow a more uniform understanding of the information contained within the report.
References:
1. Spine vol. 26, no. 5, pp E93-E113