Lateral Epicondylopathy

“Lateral epicondylopathy,” formerly “lateral epicondylitis, is a painful irritation of the common origin of the wrist extensor muscles. Lateral epicondylopathy (LE) is the most common cause of elbow pain. (1) The condition is related to repetitive wrist extension and is commonly referred to as “tennis elbow,” although the majority of those affected do not play tennis. (2)
The common extensor tendon originates on the lateral epicondyle and lateral supracondylar ridge of the humerus, and consists of the fused tendons of the extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris (from lateral to medial). Nearly all forces associated with wrist extension are funneled through this tendon onto lateral epicondyle. The supinator muscle lies deep to the common extensor group, with some fibers attaching to the lateral epicondyle. (3) The common extensor tendon, particularly the extensor carpi radialis brevis (ECRB), is relatively hypovascular, creating a tendency for injury and hypoxic degeneration. (4,5)
Pathologies
The pathogenesis of lateral epicondylopathy entails repetitive wrist extension, causing micro-tearing of the common extensor tendon, ultimately leading to a failed healing response and degeneration. (4,5) The primary site of injury is the extensor carpi radialis brevis (ECRB) tendon, 1-2 cm distal to its attachment on the lateral epicondyle. (4,6,7) While acute inflammation may accompany the earliest phase of tendon disease, it is unlikely to last more than a few days. (8) In chronic cases, inflammatory cells are absent. (2,8-11) Researchers now recognize that repetitive microtrauma does not cause inflammation, but rather a failure of the natural healing process, resulting in a disorganized pathological tendon degeneration, called “angioblastic degeneration.” (8,9,11-15) Since LE is primarily a degenerative condition, rather than a chronic inflammatory process as once hypothesized, the term “tendinitis” has been replaced with “tendonosis” or “tendinopathy.”. (8,10-14) True tendinitis is rare compared to tendinopathy. (16) A degenerated tendon may be predisposed to partial or full thickness tears as a result of ongoing strain, particularly rapid, eccentric overload. (15)
Lateral Epicondylopathy
Lateral epicondylopathy affects between 1 and 3% of the general population each year. (1,17) The condition occurs predominantly in the fourth or fifth decade and affects men and women equally. (1,18) LE strikes the dominant arm in 75% of cases. (18) LE results in an average of 12 weeks of disability in up to 30% of those workers affected. (19)
LE is a byproduct of excessive force or repetitive movement, combined with improper biomechanics and/or posture. (20,21) The primary risk factors for LE include repeated wrist extension and forearm supination/pronation. Certain occupations and activities are predisposed, including carpenters, bricklayers, seamstresses, tailors, pianists, drummers, those who shake hands excessively (politicians), and those who perform prolonged keyboard or mouse work. (22) Only 5% of lateral epicondylopathy patients participate in racquet sports (20), but among tennis players, 50-60% will be affected at some point in their career. (18) LE injuries related to tennis are thought to develop as a result of improper mechanics during backhands or serves. (23) Additional racquet-related risk factors include: using a new, heavy, or tightly strung racquet, excessive grip size, and hitting wet or heavy tennis balls. (22)
Symptoms
Symptoms often begin insidiously following overuse-type activity, without a history of specific trauma. The classic clinical presentation includes pain over the lateral aspect of the elbow. (22,25) Symptoms are typically provoked by activities that involve gripping and/or wrist extension. (25) Pain may vary from mild to sharp, severe pain that limits the simplest activities, like picking up a coffee cup. Rest may provide relief. (22) Symptoms and objective progress may be tracked on a DASH questionnaire or Patient-Rated Tennis Elbow Evaluation (PRTEE). (27)
Pain is generally localized, and clinicians should consider the possibility of peripheral neuropathy (radial tunnel syndrome) in patients whose symptoms radiate distally. Radial tunnel syndrome is entrapment of the radial nerve as it passes through the proximal forearm near the lateral epicondyle. Common sites of compression within the radial tunnel include the Arcade of Frohse, or within the supinator muscle. Research suggests that up to 10% of patients with lateral epicondylopathy have co-existent radial tunnel syndrome. (28) The similarities of lateral epicondylitis and radial tunnel syndrome can make differentiation of the two conditions challenging. The pain of radial tunnel syndrome should be more acute distally. (29) Nocturnal pain is more common in radial tunnel patients than those with lateral epicondylitis. (30)
Clinical Findings
The classic clinical findings for LE include pain on palpation of the lateral epicondyle, pain on resisted wrist extension, and pain on resisted middle finger extension. (31) Peak tenderness is located directly over, and slightly distal to, the lateral epicondyle, most specifically over the origin of the ECRB. Cozen’s test is basically wrist extension performed with the patient’s fist closed and elbow fully extended. The reproduction of pain upon this maneuver suggests lateral epicondylopathy. When Cozen’s maneuver produces pain when performed with the elbow slightly bent, the condition may be more challenging to manage. Mill’s test for LE involves passive stretching of the wrist extensors while the elbow is in extension. Resisted extension of the middle finger (resisted long finger extension test) places tensile stress on the ECRB tendon and often provokes LE symptoms. Clinicians should consider radial tunnel syndrome when this maneuver is more painful than Mill’s test.
Neurologic assessment should be performed to identify the possibility of cervical radiculopathy or peripheral neuropathy. Radial tunnel syndrome may manifest as diminished sensitivity along the dorsal aspect of the forearm and/or thumb, or weakness of thumb extension. (32,33)
Radiology
Plain film radiography is of little diagnostic value for the assessment of soft tissue disorders. (34) Radiographs may be appropriate in the presence of “red flags” or a history of trauma, to rule out fracture, dislocation, infection, or neoplasm. (34,35) Occasionally, radiographs may demonstrate calcific tendinitis or the presence of intra-articular pathology. (35) MRI has the ability to demonstrate tendinosis as well as bony or soft tissue pathology. Diagnostic ultrasound is useful for evaluating the common extensor tendon for tendinitis or tearing. (35)
The differential diagnosis of lateral epicondylopathy includes cervical radiculopathy, radial tunnel syndrome, osteoarthritis, fracture, infection, neoplasm, osteochondral loose body, elbow synovitis, triceps tendinitis, sprain/strain, myofascial pain syndrome, and inflammatory arthropathy.
Treatment
The natural course of lateral epicondylopathy can be exasperating. Twenty percent of untreated patients demonstrate no improvement after one year. (36) Even those patients undergoing optimal management may require three to four months for a full recovery. (16) Evidence supports the use of traditional conservative measures, including manipulation, mobilization, exercise, friction massage, bracing, and modalities. (38,39)
Initially, patients may require selective rest and avoidance of activities involving repetitive wrist extension, pronation, or supination. Counter-irritant creams may provide palliative relief. Ice or home ice massage may be helpful for acute “tendinitis” patients, but do little to alter the long-term course of chronic tendinopathy. Tennis players should look for ways to improve mechanics, including not leading with their elbows and switching to a 2-hand backstroke that limits pronation. (23) The use of a counter-force strap applied firmly approximately 10 cm distal to the elbow joint, has been shown to decrease pain and improve grip strength. (40-42) Counter-force braces should not be used in cases of concurrent radial tunnel syndrome, as the additional pressure will likely exacerbate compressive neuropathy symptoms. Some clinicians choose to employ a cock-up wrist splint, although this orthotic has less support in the literature. (42,43)
Mobilization
There is moderate evidence supporting the use of mobilization/manipulation of the elbow, cervical spine, and wrist for the treatment of LE. (44-54) Mobilization/ manipulation of the elbow demonstrates an immediate decrease in pain and a substantial increase in pain-free grip. (45,46,54) Various techniques are employed for restoring elbow mobility, including McKenzie Directional Therapy (MDT), Mulligan mobilization, and Mill’s manipulation, which is performed as a high-velocity thrust to the extended elbow while the wrist and hand are flexed. (55) Some studies suggest that mobilization or manipulation of the wrist may be as effective as a conventional local treatment for lateral epicondylopathy. (52,53) Manipulation of the cervical and cervicothoracic region has been shown to decrease pain and disability in lateral epicondylopathy patients. (47-49,51)
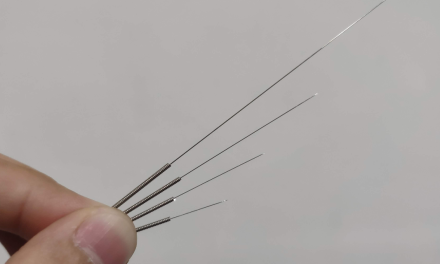
Any tendinosis is associated with excessive, disorganized collagen formation, scarring, and contracture of peritendinous tissue. (51) IASTM is thought to help mobilize scar tissue and increase pliability by re-initiating an inflammatory process through controlled microtrauma. (51,56) The use of IASTM has demonstrated “significantly better” outcomes than exercise alone, with 57% resolution of complaints after one month of care, and 78% resolution after two months. (57) Anecdotal evidence suggests that dry needling may be a useful alternative for recalcitrant cases.
Myofascial Release
Myofascial release is an effective treatment for lateral epicondylopathy. (71) STM and stretching exercises should be directed at the wrist extensors and supinator muscle. Resistance training may begin isometrically and advance to eccentric exercise. All outcome measures for the treatment of lateral epicondylopathy show improvement with the addition of eccentric wrist extensor strengthening. (43) Eccentric strengthening is thought to stimulate collagen metabolism and synthesis. (43,58) The “Tyler Twist” exercise, utilizing a Theraband Flexbar, is a novel approach to eccentric strengthening that has shown significant pain reduction and excellent outcomes in limited trials. (69,70)
Some clinicians advocate the use of low-level laser, ultrasound, phonophoresis, iontophoresis, elastic therapeutic tape and acupuncture for the treatment of lateral epicondylopathy. (38,43) More recent concepts for the management of LE include the application of a glycerol trinitrate patch, which has been shown to decrease pain and enhance healing while stimulating collagen synthesis. (43,59)
Medical Management
Medical management includes the use of oral or topical NSAIDs. (43,60) Autologous or platelet-enriched-plasma (PRP) injections have been advocated for the treatment of lateral epicondylopathy (61), but remain unproven. (62,63) While corticoid steroid injections may provide some short-term benefit, these injections can be detrimental to long-term recovery. (64) One study demonstrated that corticosteroid injections significantly reduce pain, with 78% success at six weeks (versus 65% improvement for standard physical therapy.) (65) Unfortunately, the same study demonstrated that at one year, those patients treated by injection were “significantly worse,” compared to those managed conventionally or those who underwent no treatment. (65)
Less than 11% of patients will require surgical intervention. (36) Factors associated with a poor prognosis for conservative care include heavy manual labor, lateral epicondylopathy in the dominant arm, high pain perception, and poor coping strategies. (36) Ultrasound-guided percutaneous radiofrequency thermal lesioning (RTL) is a minimally-invasive surgical procedure used to stimulate healing. Studies regarding RTL management of LE demonstrate significant pain reduction and grip strength improvement, with 85% of patients reporting pain relief after one month, and 91% reporting good to excellent satisfaction after six months. (66) Surgical intervention, including arthroscopic removal of the pathologic tendon tissue, has demonstrated success, but should only be considered after six months of failed conservative care. (67)
References:
1. Bigorre N, Raimbeau G, Fouque P-A, Saint Cast Y, Rabarin F, Cesari B. Lateral epicondylitis treatment by extensor carpi radialis fasciotomy and radial nerve decompression: Is outcome influenced by the occupational disease compensation aspect? Orthopaedics & Traumatology: Surgery & Research. 2011; 97(2): 159-163
2. Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomized trial. BMJ. Nov 4 2006;333(7575):939.
3. Erak S, Day R, Wang A. The role of the supinator in the pathogenesis of chronic lateral elbow pain: a biomechanical study. J Hand Surg (Br) 2004;29(5):461–464.
4. Altan L, Kanat E. Conservative treatment of lateral epicondylitis: comparison of two different orthotic devices. Clin Rheumatol. Aug 2008;27(8):1015-9.
5. Walz DM, Newman JS, Konin GP, Ross G. Epicondylitis: Pathogenesis, imaging, and treatment. RadioGraphics. 2010;(30):167-183.
6. Conway JE. Clinical evaluation of elbow injuries in the athlete. J Musculoskeletal Med. 1998;15(10):43–52.
7. Rettig AC. Elbow, forearm, and wrist injuries in the athlete. Sports Med. 1998;25(2):115–130.
8. Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth. BMJ. 2002;324(7338):626–627.
9. Boyer MI, Hastings H. Lateral tennis elbow: “Is there any science out there? J Shoulder Elbow Surg. 1999;8(5):481–491.
10. Regan W, Wold LE, Conrad R, Morrey BF. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med. 1992;20:746.
11. . Kraushaar BS, Nirschl RP. Tendonosis of the elbow (Tennis Elbow). Clinical features and finding of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81:259–278.
12. Ollivere CO, Nirschl RP. Tennis elbow: current concepts and rehabilitation. Sports Med. 1996;22(2):133–139.
14. Nirschl RP. Elbow tendonosis/tennis elbow. Clin Sports Med. 1992;11:851–870.
15. Bishai SK, Plancher KD. The basic science of lateral epicondylosis: Update for the future. Techniques in Orthopaedics. 2006;21(4):250-255.
16. Khan, K.M., Cook, J.L., Taunton, J.E., et al., 2000. Overuse tendinosis, not tendonitis. Part 1: a new paradigm for a difficult clinical problem. Physics and Sportsmedicine 28, 38–48.
17. Hong QN, Durand MJ, Loisel P. Treatment of lateral epicondylitis: where is the evidence? Joint Bone Spine. 2004;71(5):369–373
18. Ollivere CO, Nirschl RP. Tennis elbow: current concepts and rehabilitation. Sports Med. 1996;22(2):133–139
19. Verhaar JA. Tennis elbow. Anatomical, epidemiological and therapeutic aspects. Int Orthop. Oct 1994;18(5):263-267.
20. Haahr JP, Andersen JH. Physical and psychosocial risk factors for lateral epicondylitis: a population based case-referent study. Occup Environ Med. 2003;60(5):322-329.
21. Bernard B. Musculoskeletal Disorders (MSD) and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. Cincinnati, OH: NIOSH, Centers for Disease Control and Prevention National Institute for Occupational Safety and Health; 1997.
22. Walrod BJ. Lateral Epicondylitis Clinical Presentation Emedicine accessed: 04/29/2014 http://emedicine.medscape.com/article/96969-clinical
23. Loftice J, Fleisig GS, Zheng N, Andrews JR. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23(4):519–530.
25. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: Current concepts. J Am Acad Ortho Surg .2008;(16):19-29
27. Rompe JD, Overend TJ, MacDermid JC. Validation of the patient-rated tennis elbow questionnaire. J Hand Ther. 2007;20(1):3-10
28. Spinner M, Spinner RJ. Management of nerve compression lesions of the upper extremity. In: Management of Peripheral Nerve Problems, 2nd ed. 1998, Philadelphia, WB Saunders, pp. 501-533.
29. Lister GD, Belsole RB, Kleinert HE. The radial tunnel syndrome. J Hand Surg [Am].1979; 4:52–59
30. Hammer W. Is it Tennis Elbow or Radial Tunnel? Dynamic Chiropractic – December 29, 1997, Vol. 15, Issue 26
31. Tyler TF, Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: A prospective randomized trial J Shoulder Elbow Surg (2010) 19, 917-922
32. Theodore T. Miller, William R. Reinus. Nerve Entrapment Syndromes of the Elbow, Forearm, and Wrist. AJR 2010; 195:585 –594
33. Kirici Y, Irmak MK: Investigation of two possible compression sites of the deep branch of the radial nerve and nerve supply of the extensor carpi radialis brevis muscle. Neurol Med Chir (Tokyo) 2004, 44:14-18.
34. Steinbach L, Dalinka M, Alazraki M. Chronic elbow pain. Reston, VA: American College of Radiology; 2001.
35. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: Current concepts. J Am Acad Ortho Surg .2008;(16):19-29
36. Janssen S, De Smet L. Responsiveness of the DASH questionnaire for surgically treated tennis elbow. Acta Chir Belg. 2008;108(5): 583-585.
37. Assendelft WJ, Hay EM, Adshead R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic overview. Br J Gen Pract. Apr 1996;46(405):209-16.
38. Mark T Pfefer , Stephan R. Cooper, and Nathan L.Uhl Chiropractic Management Of Tendinopathy: A Literature Synthesis. J Manipulative Physiol Ther 2009;32:41-52
39. Waugh EJ, Jaglal SB, Davis AM, Tomlinson G, Verrier MC. Factors associated with prognosis of lateral epicondylosis after 8 weeks of physical therapy. Arch Phys Med Rehabil 2004;85:308-18.
40. Altan L, Kanat E. Conservative treatment of lateral epicondylitis: comparison of two different orthotic devices. Clin Rheumatol. Mar 26, 2008; epub ahead of print.
41. Borkholder CD, Hill VA, Fess EE. The efficacy of splinting for lateral epicondylitis: a systematic review. J Hand Ther. Apr-Jun 2004;17(2):181-99.
42. Jafarian FS, Demneh ES, Tyson SF. The immediate effect of orthotic management on grip strength of patients with lateral epicondylosis. J Orthop Sports Phys Ther. Jun 2009;39(6):484-9.
43. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: Current concepts. J Am Acad Ortho Surg .2008;(16):19-29
44. Souza T. Differential Diagnosis and Management for the Chiropractor. 2009. Edition 4.
45. Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and metaanalysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. Jul 2005;39(7):411-422; discussion 411-422.
46. Vicenzino B, Paungmali A, Buratowski S, Wright A. Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Man Ther. Nov 2001;6(4):205-212.
47. Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: a pilot clinical trial. J Man Manip Ther 2005;13:143-51.
48. Cleland JA, Whitman JM, Fritz JM. Effectiveness of manual physical therapy to the cervical spine in the management of lateral epicondylalgia: a retrospective analysis. J Orthop Sports Phys Ther 2004;34:713-22.
49. Josué Fernández-Carnero, Cesar Fernández-de-las-Peñas, Joshua A. Cleland, Immediate Hypoalgesic and Motor Effects After a Single Cervical Spine Manipulation in Subjects With Lateral Epicondylalgia Journal of Manipulative and Physiological Therapeutics Volume 31, Issue 9, November–December 2008, Pages 675–681
50. Javier González-Iglesias, Joshua A. Cleland, Maria del Rosario Gutierrez-Vega, and Cesar Fernández-de-las-Peñas, Multimodal Management Of Lateral Epicondylalgia In Rock Climbers :A prospective Case Series J Manipulative Physiol Ther 2011;34:635-642
51. Hammer WI. The effect of mechanical load on degenerated soft tissue. Journal of bodywork and movement therapies 08/2008; 12(3):246-56.
52. Manchanda Geetu, Lecturer, Grover Deepak Effectiveness of movement with mobilization compared with manipulation of wrist in case of lateral epicondylitis. Indian Journal of Physiotherapy and Occupational Therapy – An International Journal, 2008, Volume: 2, Issue: 1 16-25
53. Peter AA Struijs, Pieter-Jan Damen, Eric WP Bakker, Leendert Blankevoort, Willem JJ Assendelft and C Niek van Dijk Manipulation of the Wrist for Management of Lateral Epicondylitis: A Randomized Pilot Study Physical Therapy July 2003 vol. 83 no. 7 608-616
54. Nirschl RP. Elbow Tendonosis/ Tennis elbow. Clin Sports Med. 1986;5: 638-644
55. Cyriax J. Cyriax’s Illustrated Manual of Orthopaedic Medicine. 2nd ed. Butterworth Heinemann: Oxford, UK; 1983.
56. Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study.
57. Stover S, Sevier T, Helfst R, Jansen CWS. The effectiveness of the ASTYM system in improving treatment outcomes in patients with lateral epicondylitis: a single-blinded randomized trial. Joint #1. Presented at the Joint Annual ASSH/ASHT Meeting. Sept. 22-24, 2005. San Antonio.
58. Langberg, H., Ellingsgaard, H., Madsen, T., et al., 2007. Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scandinavian Journal of Medicine and Science in Sports 17, 61–66
59. Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow: a randomized, double-blinded, placebo-controlled clinical trial. Am J Sports Med. Nov-Dec 2003;31(6):915-20
60. Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomized trial. BMJ. Nov 4 2006;333(7575):939.
61. Connell DA, Ali KE, Ahmad M, Lambert S, Corbett S, Curtis M. Ultrasound-guided autologous blood injection for tennis elbow. Skeletal Radiol. Jun 2006;35(6):371-7
62. Behrens SB, Deren ME, Matson AP, Bruce B, Green A. A review of modern management of lateral epicondylitis. Phys Sportsmed. 2012;40(2): 34-40.
63. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. American Journal of Sports Medicine. 34;(11):1774-1778
64. PM&R Knowledge Now. Epicondylosis (lateral) with and without nerve entrapment. Accessed 5/12/14 from aapmr.org
65. Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomized trial. BMJ. Nov 4 2006;333(7575):939.
66. Lin CL, Lee JS, Su WR, Kuo LC, Tai TW, Jou IM. Clinical and Ultrasonographic Results of Ultrasonographically Guided Percutaneous Radiofrequency Lesioning in the Treatment of Recalcitrant Lateral Epicondylitis. Am J Sports Med. Aug 11, 2011
67. Baker CL Jr, Baker CL 3rd. Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med. Feb 2008;36(2):254-60
68. Smidt N, Assendelft WJ, Arola H, et al. Effectiveness of physiotherapy for lateral epicondylitis: a systematic review. Ann Med. 2003;35(1):51-62
69. Page P. A New Exercise For Tennis Elbow That Works! N Am J Sports Phys Ther. Sep 2010; 5(3): 189–193.
70. Tyler T.F., et al. , Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: A prospective randomized trial. J Shoulder Elbow Surg. 2010; 19(6):917–922
71. Piper S, Shearer HM, Côté P, Wong JJ, Yu H, Varatharajan S, Southerst D, Randhawa KA, Sutton DA, Stupar M, Nordin MC, Mior SA, van der Velde GM, Taylor-Vaisey AL. The effectiveness of soft-tissue therapy for the management of musculoskeletal disorders and injuries of the upper and lower extremities: A systematic review by the Ontario Protocol for Traffic Injury management (OPTIMa) collaboration. Man Ther. 2016 Feb;21:18-34.