Essentials of a Radiology Report for the Chiropractic Physician

Radiography continues to be the most often utilized imaging modality in health care, particularly amongst chiropractic physicians. Many chiropractic physicians choose to utilize the interpretation services of a chiropractic radiologist (DACBR), but many also choose to interpret the x-rays of their patients themselves. It is important to understand that the interpreting physician is responsible for everything visible on the radiograph — not exclusively the postural and/ or listing findings — and is assuming the same expertise as a radiologist. Additionally, if the doctor is billing the patient’s insurance for the technical and professional component of the x-ray, it is vital that the doctor generate a report for those radiographs. While it is considered acceptable to include in your patient notes the information that would normally be found in a typical radiography report, a separate report is more useful when comparing to previous or future studies and providing the information to other medical professionals.
The purpose of the radiology report is to be the permanent record of the radiographic findings and diagnoses. Yochum and Rowe1 discuss several important reasons for recording radiographic findings:
- providing an accurate means of recording findings for use during comparison with previous or later examinations;
- serving as documentation in medicolegal circumstances;
- providing a permanent record in case the radiographs are lost or not immediately available;
- offering a means of communication with other practitioners and health professionals; and
- expediting the management regime by providing a summary of important indications and contraindications for therapy.
The structure of the report is important, in that it helps organize the required information into an understandable format, as well as creating a consistent habit for the practitioner and therefore avoids missing documentation of any component. A standard radiology report (figure 1) should include the following:
- Preliminary information
- Radiologic findings
- Impression
- Recommendations (if applicable)
- Signature
Figure 1 – Sample Radiology Report
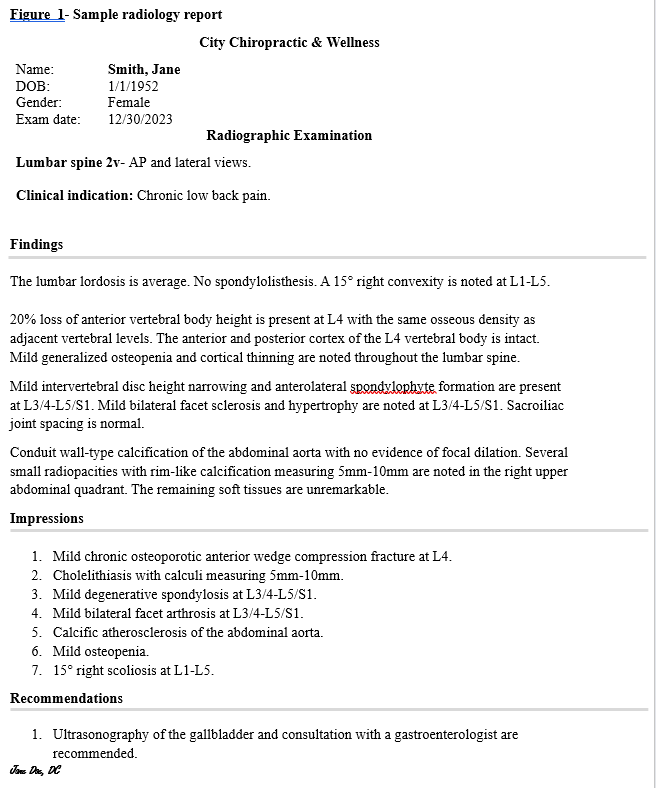
Preliminary information should include the patient’s name, date of birth, date of study, date of report, and views taken. The preliminary information should also include pertinent clinical information and indication for the study. If the radiographs are sent to a radiologist for review and interpretation, be sure to include pertinent historical information, such as chief complaint, specific concerns, and history of malignancy, trauma, or surgery. A radiologist cannot perform his/her job properly if left in the dark regarding patient history, which can lead to excessive widening of diagnostic considerations and possible unnecessary imaging or referral recommendations.
Radiologic findings are written as a paragraph form narrative of the descriptive radiographic observations. These findings should follow a systematic evaluation of the alignment, bone, cartilage, and soft tissue structures (ABCS). Each component should be discussed with pertinent negatives included. The ABCS pattern is often used, as it is a good way to make sure that each component is evaluated in every case, but the order is really the choice of the doctor — just make sure to follow the same order each time. If prior radiographs are available, comparison should be discussed, such as changes in measurements, increased degenerative changes, etc.
- Alignment- This section includes, but is not limited to, any pertinent measurements, angles, convexity, postural information, and anterolithesis/ retrolisthesis.
- Bone- This section should discuss any presence of fracture, osseous lesions (tumor, infection), and presence of osteopenia.
- Cartilage- Because we cannot actually “see” cartilage on x-ray, this section focuses on the joint spaces in which the cartilage is located. This includes joint space symmetry, joint space loss or widening, presence of osteophytes, erosive changes, and the presence of cartilaginous calcification.
- Soft tissue- This section describes the shadows formed by solid organs, gas located in the bowel, possible airway disease, and calcifications of the soft tissue structures such as vascular calcification or mass calcification. This section will also discuss abnormal fat pad displacement, soft tissue edema, any abnormal mass, or any abnormal finding involving the soft tissue structures. Normal physiologic calcifications such as costochondral calcification or thyroid cartilage calcification should not be included.
Impressions are the summary of the findings written in a concise point-by-point numbered list (Table 1). Impressions should be listed in order of importance, rather than follow the ABCS method. Each impression should sum up the important findings in a diagnosis or a list of differential diagnoses (if applicable). Not all impressions require a list of diagnostic possibilities, and considerations should include the most likely diagnoses based on findings and historical/ clinical data.
Recommendations are required when further imaging, testing, or referral are required. This section should NOT include treatment recommendations.
Signature should be included at the end of the report and be dated on the date of report generation.
Table 1- Example of findings with correlative impressions and recommendations
Category Findings Impressions Recommendations Alignment A 25% anterior translation of L5 vertebral body relative to S1 is present. Grade 1 spondylolisthesis. Bone A well-defined radiolucent centrally located lesion with punctate calcification measuring 3-cm in greatest diameter is noted within the proximal humeral metaphysis. Well-defined radiolucent lesion with punctate calcification is most consistent with a benign enchondroma or, less likely, medullary infarction or low-grade chondrosarcoma. Contrast-enhanced MR imaging is recommended if symptoms are present clinically. Cartilage Coarse, triangular calcification of the medial meniscus is present. Calcium pyrophosphate dihydrate deposition disease. Referral to rheumatologist is recommended. Soft tissue Conduit-wall type calcification of the abdominal aorta is noted with a focal 3.5-cm dilation at the level of L2. 3.5-cm abdominal aortic aneurysm. Ultrasonography of the abdominal aorta is warranted.
In conclusion, the radiology report is a vital component of the patient chart that should not be ignored or a mere checklist in the file. The x-rays themselves are not enough to achieve the proper standard of care for the patient or adequate record keeping. The report is a permanent record of the objective findings and correlative impressions that the doctor utilizes to correlate clinically and determine appropriate care. The report should be as concise as possible, with care taken to ensure all findings are discussed and considered.
References
Yochum TR, Rowe LJ. Essential of Skeletal Radiology Volume 3. Baltimore; Lippincott Williams & Wilkins, 2005: 1547.
Hartung M, Bickle I, Gaillard F, and Kanne J. How to Create a Great Radiology Report.
RadioGraphics 2020; 40(6): 1658-1670.
Taylor J. Writing radiology reports in chiropractic. JCCA March1990; 34(1): 30-34.