
Chronic Pelvic Pain
Persistent pelvic pain for six (6) months or more is considered to be chronic and it is one of the most common reasons that women seek care in a primary care practice. The etiology may include PID, endometriosis, various diseases of the uterus and adnexae, urinary tract problems, bowel disease or musculoskeletal disorders. Many women continue to have pain, even when no specific diagnosis can be established. Chronic pelvic pain can be and usually is frustrating for the physician and the woman. The frustration often results in frequent visits to a variety of physicians, numerous diagnostic studies, all too frequent pelvic surgery and many times a hysterectomy without resolution.
History
The woman should be permitted to describe her pain in relation to such potential precipitating factors as her menstrual cycle, intercourse and stress. She should be questioned concerning pain in other parts of her body such as headaches, backaches, etc. The menstrual history often reveals abnormal uterine bleeding in a pattern that may be consistent with pelvic pathology. Her sexual history may reveal significant dyspareunia and a history of a pelvic infection may suggest an inflammatory condition or possibly adhesions. A musculoskeletal condition could very well be at the root of the problem.
The woman should be encouraged to discuss past problems of other organ systems, especially the urinary and gastrointestinal systems. If she has a history of pelvic or abdominal infection and/or surgical or diagnostic procedures you may suspect an occult infection, inflammation or adhesions. It may also prove prudent to question the woman concerning her current and past marital status; number of children, if any; stress as a child, adolescent or adult; and any instances of physical or sexual abuse.
Physical Examination
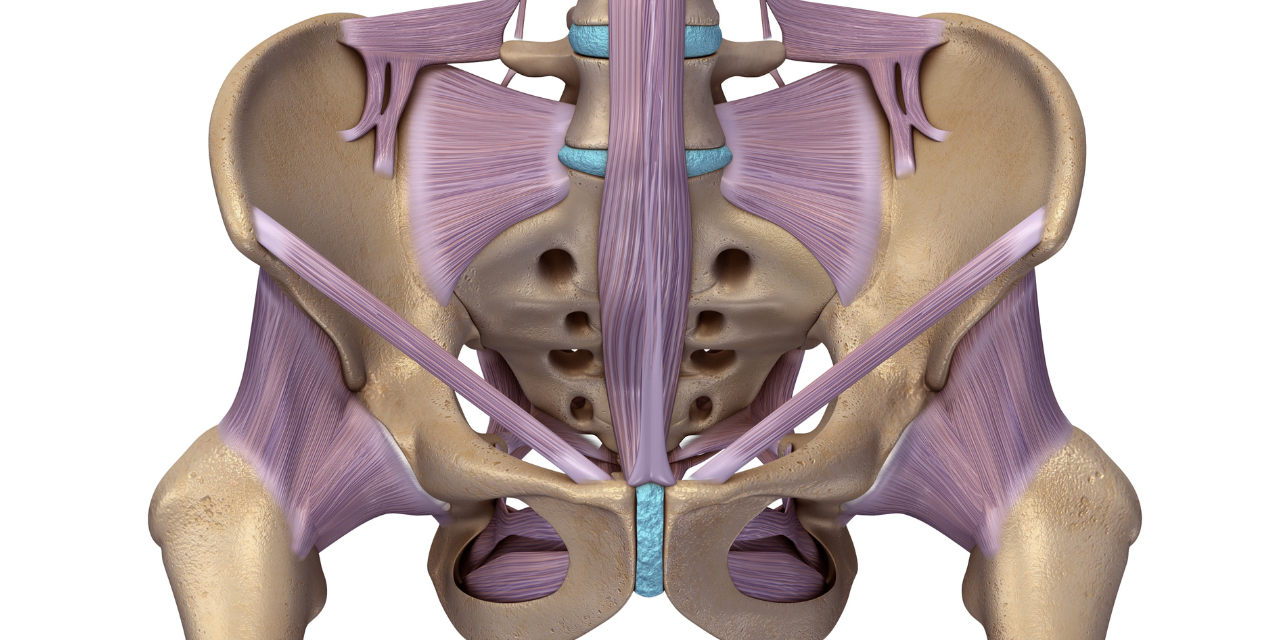
During the examination, the physician should note any abdominal or pelvic scars that might indicate previous injury, infection or surgery. A complete pelvic examination should be performed and vaginal and cervical cultures should be performed to rule out an infection with discharge or an occult infection. The pelvic floor supports should be carefully evaluated for laxity or unusual firmness as some chronic pelvic pain may be caused by uterine prolapse, cystocele, rectocele or enterocele. The uterus and adnexae should be carefully evaluated for position, size, mobility and any evidence of tenderness, masses or irregularities. Any nodularity along the uterosacral ligaments or cul-de-sac should be noted as these may suggest pathology, endometriosis or neoplasia. Should the physician find any indication of GI or urinary tract pathology further evaluation of these systems is obviously warranted.
The following laboratory tests should be performed on any woman with chronic pelvic pain:
- Vaginal and cervical cultures.
- Chem screen.
- CBC with diff.
- Thyroid profile which includes a T3, T4, and Free T4.
- ESR.
- VDRL.
- Pap smear.
- Urinalysis, possibly a urine culture.
- Possibly ELISA/ACT food and chemical allergy testing.
Imaging Studies
If the woman has an abnormal pelvic exam, a pelvic ultrasound may be able to more clearly delineate the presence of uterine or adnexal pathology. Any abnormal findings on the pelvic ultrasound may be further delineated with an MRI of the pelvis. Even if the pelvic examination is unremarkable these studies may be helpful in identifying a problem. The physician should keep in mind that laparoscopic procedures are typically performed by allopathic physicians, but Cunanan and colleagues found that these are frequently negative. Also, any surgical procedure results in scar tissue which may itself be the cause of future chronic pelvic pain. In those laparoscopies which did identify a problem adhesions were the most common cause followed closely by endometriosis. It should be noted that no follow-up study was performed to determine if the chronic pelvic pain was resolved by these laparoscopic procedures.
Beard and colleagues have made a case for the possibility that the existence of a “pelvic congestion syndrome” may be the cause of chronic pelvic pain. They performed pelvic venograms on women with chronic pelvic pain and found that the women with no obvious pathology exhibited definite increases in diameter of and slower emptying times in the ovarian veins compared with groups of women who had no pelvic pain.
The physician must be careful not to discredit the possibility of an underlying psychological problem. Gross and colleagues found that women suffering from chronic pelvic pain were more likely than without pelvic pain to have a history of physical, sexual and drug abuse, unemployment, and various mental health disorders. A psychiatric evaluation of their women found that most of these women fell into one of three categories:
- Borderline personality disorder.
- Depressive disorders.
- Somatization problems.



















