
Burning Pain in My Chest – Heartburn
Heartburn
Three patients walked into my office this week complaining of heartburn. This turns out to be a very common complaint when going through a patient’s medical history in a nutrition-based practice. It could also be a very common complaint in musculoskeletal practice, as the incidence of heartburn is very high. About one-third of Americans have heartburn at least once a month, with 10% experiencing it nearly every day, according to Harvard Medical School. That burning pain in your chest is often worse after eating, in the late hours or when lying down or bending over. It is a very common symptom; however, it is not normal to have. There is definitely something wrong if you have this pain.
GERD
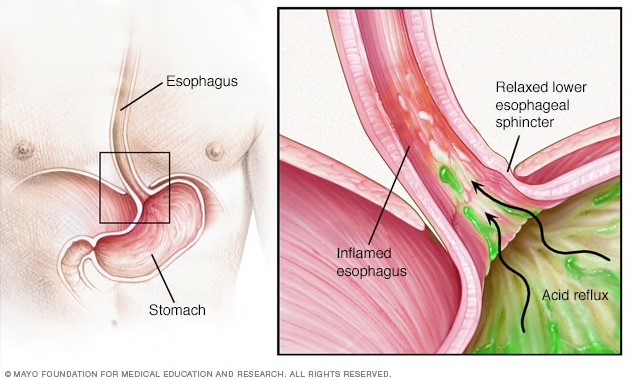
If it interferes with your daily life or it occurs consistently, it is often referred to as GERD. Patients may also describe a bitter or acidic taste in their mouth, in addition to the burning sensation in their chest. Typically, when we eat food and we chew, we release digestive enzymes in our saliva to help break down the food. Theoretically, we are supposed to chew to the point that food is more like the consistency of a liquid. Once that is done, the food moves down the esophagus into the stomach through a sphincter. Anatomically, a band of muscle around the lower part of the esophagus (lower esophageal sphincter or LES) relaxes to allow the food and liquid to go into the stomach, and then it tightens again. If the LES relaxes abnormally or weakens, the stomach acid can flow back up into the esophagus and cause the burning sensations, because the acid irritates the esophageal lining, which we then call heartburn. If we don’t chew enough or we don’t have enough enzymes in our saliva, this can inhibit the proper breakdown of food, thus contributing to the symptoms. If the food gets to the stomach and the digestive process is hindered by a lack of enzymes, then occasionally the food can regurgitate back up into the esophagus, causing the burning.
The acid from the stomach doesn’t belong in the esophagus, which causes the burn sensation, whereas in the stomach the burn is not felt. It is also possible that a patent doesn’t have enough acid or HCL in the stomach to continue the digestive process, also contributing to the food ascending where it doesn’t belong.
Triggers
There are many triggers including spicy foods, onions, citrus, tomatoes, fatty and fried foods, peppermint, chocolate, alcohol, carbonated drinks, caffeine, fatty meals or just over-consuming foods. Food sensitivities may also trigger a reaction by increasing an inflammatory response. Excess weight or pregnancy may also increase the risk of heartburn.
Lowering levels of stress can positively influence a decrease in heartburn. Encouraging a patient to work on intention breathing, meditation, or yoga is a great place to start.
Check the medications your patients are taking, as well, because some are known to be contributors to this condition. NSAIDs, antibiotics, calcium channel blockers, osteoporosis drugs, inhalers, Bentyl, antidepressants such as Elavil, hormones such as Promethium and Tibolone, erectile dysfunction meds like Viagra, opioids, some diabetes drugs, and some sedatives can be the cause of the heartburn.
Drugs
There are three main classifications of drugs commonly recommended for heartburn/GERD. Acid neutralizers such as Tums, Rolaids, Maalox, Alka Seltzer, and Mylanta only last for a short period and are not a permanent fix. H2 Blockers are the second and attempt to reduce the production of stomach acid; however, we still want stomach acid, we just don’t want it in the esophagus. The effects take a bit longer to work but last a little longer than acid neutralizers. Proton pump inhibitors are the third type of medication. Prevacid, Nexium, Omeprazole, and Prilosec completely block the production of stomach acid and can last up to 72 hours.
This seems counterintuitive when stomach acid is needed for the digestive process. The acid helps create a barrier to protect against various pathogens as well. With decreased stomach acid, the risk of nutritional deficiencies also goes up. We are creating the potential for additional problems by fixing one inappropriately. Wouldn’t it be better to eliminate the cause of the heartburn, rather than shut off the production of acid that when used properly has a specific function that isn’t harmful? Some of these medications cause more side effects. Just this week, Zantac, a popular OTC heartburn drug was pulled off the market because the company announced it contains low levels of a substance called NDMA that can cause cancer. GERD can eventually damage the esophagus which can lead to chronic inflammation and precancerous changes or Barrett’s esophagitis. Now if we add meds with chemicals, we can potentially increase that risk.
Supplementation
In a nutrition-based practice, we have a different approach. For symptoms, supplementation can provide a lot of relief. Supplements you can recommend with confidence will include: Digestive enzymes taken 1-2 hours before eating a meal, HCL with pepsin 650 mg with each meal, L-glutamine 2-6g twice a day with meals, and probiotics daily. Licorice, Devil’s Claw, bromelain, papaya, barberry, slippery elm and marshmallow, and chamomile, either by themselves or in combination products, can also be very beneficial for your patients, without causing any significant side effects. Addressing the underlying cause of replenishing enzymes, increasing stomach acid, or healing the intestinal lining and reducing inflammation can have a long term effect.
When symptoms kick in, a quick fix might just be that teaspoon of baking soda. Sodium bicarbonate has a high pH, which can help neutralize the stomach acid that moves up, causing the burning sensation. Just mix it in 8 ounces of water, and drink it. Be careful not to use it too often, or it might cause swelling or nausea due to raising sodium levels. Aloe vera juice can also be extremely soothing. Half a cup has been known to reduce inflammation but is also a laxative, so don’t be surprised if your constipation is also eliminated.
Too Little Acid
If the cause is a lack of acid in the stomach, then apple cider vinegar can help regulate the LES by keeping it tight. Use three teaspoons of organic unfiltered in 8 ounces of water before a meal, before bedtime, or, if severe, a few extra times during the day may help. If it makes it worse, it is an indication that your heartburn is not an indication of too little stomach acid. Smoking and drinking alcohol are other contributing factors. Both will weaken your LES, allowing more movement upward.
Some other fun foods that can neutralize the symptoms include a teaspoon of yellow mustard, a small handful of almonds after a meal, ginger root tea, banana, and apples. These can be quick home remedies until your patient gets on the appropriate supplementation or limit the known triggers. Small meals, eating 3 hours before lying down at night, and healthier food choices will also lead to greater success for those affected.
Think about how many lives you can affect in your practice by just addressing this one very common symptom.
References
Drugs.com
de Bortoli N1, Martinucci I1, Savarino E2, Franchi R1, Bertani L1, Russo S1, Ceccarelli L1, Costa F1, Bellini M1, Blandizzi C3, Savarino V4, Marchi S1. Lower pH values of weakly acidic refluxes as determinants of heartburn perception in gastroesophageal reflux disease patients with normal esophageal acid exposure.
Dis Esophagus. 2016 Jan;29(1):3-9. doi: 10.1111/dote.12284. Epub 2014 Sep 12.Gastroenterology. 2017 Mar;152(4):706-715. doi: 10.1053/j.gastro.2017.01.031.
Freedberg DE1, Kim LS2, Yang YX3. Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. https://www.ncbi.nlm.nih.gov/pubmed/28257716#



















