
Athletic Trainers and DCs

I’ve recently seen some posts that concern me in chiropractic forums on social media. Largely the context of these posts is negative and often misinformed. Typically, the posts ridicule athletic trainers. In some cases, the critique is pointed toward a specific athletic trainer. Fair enough. Every profession has a spectrum of great to not-so-great. In other cases, the negative critique is pointed towards the profession at large. These posts are misinformed.
I have a unique vantage point as a dual-credentialed athletic trainer and chiropractic physician. I’ve worked both sides of the relationship. I’ve failed, succeeded and learned so much over the past 19 years in health care.
The goal of this article is to give you a different perspective. Hopefully, that perspective will help in forming outstanding professional relationships with certified athletic trainers (ATCs). At the very least, I hope you’ll consider a different perspective. I hope the tidbits on the relationship-building benefit your athletes, your community, the ATCs with whom you work with and your practice.
From the Outside Looking In
Student trainers and certified athletic trainers often do not have much exposure to chiropractic physicians. This is a harsh reality is that is a BIG obstacle towards building the ATC-DC relationship.
From the start, the athletic training curriculum is housed within the university setting. The university settings consist of large, accredited 4-year institutions with a multitude of degrees, contrasted with the small, professionally-focused chiropractic college setting with enrollments of 2,000 students or less. The large 4-year institutions often have allied health programs, such as physical therapy, occupational therapy, and medicine. At the very least, these academic institutions have pre-med, pre-PT, or other programs tailored towards entry into medical or other allied health programs. Relationship-building and cross-training with future professionals begin early. Chiropractic physicians are on the outside looking in when these relationships begin.
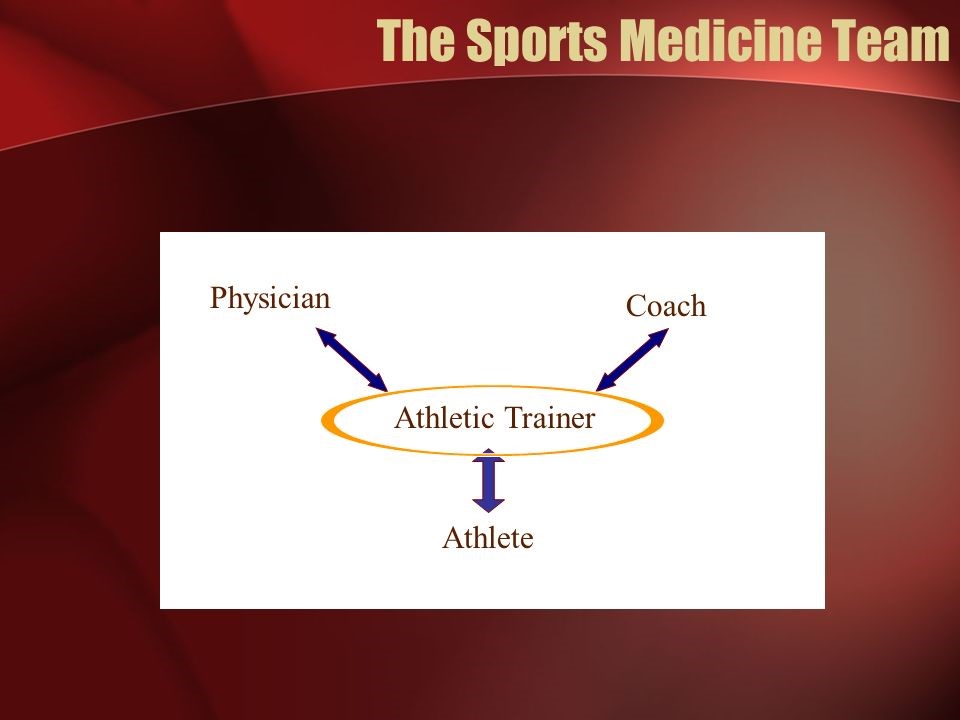
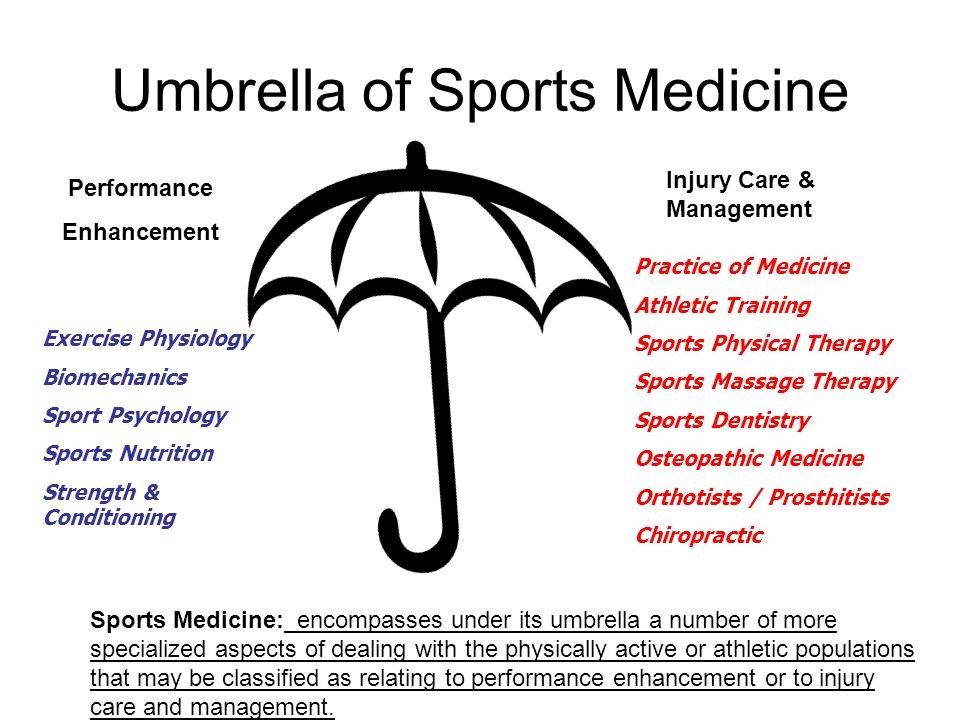
Utilizing the sports medicine team is part of standard training within the athletic training curriculum. Daily interactions come with athletes and coaches in all settings. Daily contact also occurs with equipment managers and strength coaches in larger settings. Periodic interactions occur with the team physician(s), other medical specialists, physical therapists, nutritionists, dentists, massage therapists, acupuncturists or other specialty personnel depending on the setup. The ATC is at the center of it all, though.
Integrated Settings
Larger settings typically have robust sports medicine teams with frequent contact and communication. Professional teams, Olympic athletes and high-level college sports teams have a more integrated setting, exchanging the athlete from one provider to the next in a seamless fashion. Settings like high school sports or youth sports almost certainly will feature less contact with members of the sports medicine team. Smaller settings effectively place the athletic trainer on an “island.”
From the Outside Looking in
This is the ATC to DC perspective. From the outside looking in, many athletic trainers have no idea that a subset of the profession treats sports injuries. ATCs have not worked side by side on the sidelines with DCs. ATCs have not seen you in their training room. ATCs have not taken college coursework or post-graduate continuing education courses with DCs. ATC training from its inception is heavily biased towards allopathic medicine and the allied health model. Remember, training is often housed within the standard 4-year university setting with coursework and experiences geared towards developing relationships with the immediate support staff, team orthopedist and team physician.
DCs have a lot of ground to make up before the ATC will even let them in. Using a sports analogy, you are in the later stages of a baseball game and you are trailing by 3 runs. It may be difficult to get the win, but not impossible.
The difficult part is starting the ATC-DC relationship with obstacles in the way. Some of these obstacles were created long before you, the DC, came into the picture. Some of those obstacles are based on historical educational training and the role of the ATC. Some of those obstacles were also created by the transgressions of past generations of chiropractors.
I would not let a provider near my athletes unless I knew, liked and trusted him or her as an ATC. The most cherished thing an ATC can possess is trust. Violating that trust with an inept chiropractor isn’t worth the risk. It’s a bit of a harsh reality to some DCs that it will take some work to make this relationship flourish. Caveat Emptor – “Buyer Beware!” Be willing to overcome some obstacles. Be willing to put in the work!
From the Inside Looking Out
As a DC looking to forge relationships with ATCs, you’ll ask yourself the question, “Is this really worth it?” I can’t answer that question for you. I can provide some of the key pieces in creating professional understanding.
DCs are unique as professional doctorate-level portal-of-entry providers, in that for many years we were on the outside looking in. We had a poorly acknowledged and defined role within health care. Lack of mainstream integration and lack of cultural awareness historically has placed many DCs on an island. Those barriers are changing, albeit slowly. Professional isolation includes things like our terminology, philosophy, our traditional and stereotypical business model and our lack of integrated, interdisciplinary training.

ATCs are trained to operate on an island, if necessary in a small school setting, as well as to “play nicely in the sandbox” as part of the sports medicine team in larger, more integrated settings. Playing nicely in an integrated setting is foreign to many DCs, because the DC traditionally would serve the dual role of physician and small business owner.
The DC is typically the authoritarian figure of the office. ATCs by training and position are the authority figures in their training rooms but recognize the training room is a small part of the bigger picture. The disconnect in roles can lead to quite a bit of frustration when the DC tries to gain entry to the sports medicine team.
Many DCs simply aren’t aware that the training room and playing field are typically the ATC’s domain. They don’t defer appropriately to the ATC’s expertise leading to conflict. A large part of this conflict is a failure to understand, appreciate and communicate roles.

ATCs wear many hats. It takes a special person to balance these roles and wear all these hats. ATCs do the stereotypical activities of assessing injuries, enacting emergency plans, taping athletes, rehabbing athletes, making return-to-play decisions and more. ATCs deal with mundane things like filling water bottles, prepping ice chests, looking over the practice fields for potholes, filling out budget requests or checking for inclement weather. ATCs also deal with demanding coaches, parents, athletic directors or athletes.
Some ATC work weeks, depending on the context, are 60-80 hours long in the season. Athletic trainers get tired, fatigued and sometimes impatient. When you approach an ATC about helping his or her athletes, be aware of the following:
1. Strike one:
You could be dealing with a stressed-out professional who’s overworked, underpaid and poorly appreciated.
2. Strike two:
Athletic Trainers may have a preconceived notion of the stereotypical chiropractor, based on DC professional isolation, lack of interdisciplinary co-training, lack of communication about roles/responsibilities and competing financial interests.
3. Strike three:
The DC comes into the relationship with something to prove. This could be ego. This could also be an attempt by the DC to validate his or her expertise or physician status. Either way, trying to prove something comes across as abrasive to ATCs on their turf. Abrasiveness is the nail in the coffin!
Many DCs don’t even realize the deck is stacked against them. Many DCs don’t realize they could be behind by two strikes. It may seem like a harmless thing trying to prove yourself to the rest of the team, but that could rub the ATC and team the wrong way. Strike 3, and game over.
The best way of going after this is SERVICE! The DC needs to build trust. Humble service builds trust better than any other action. Serve the athletes. Serve the athletic trainers. Serve the coaches. Serve the staff. Serve the community. Serve the sports medicine team. Listen first, serve, then speak. Your humble service opens the door, not your title, skill set, expertise or even monetary donations.
Tips For Forging Outstanding DC-ATC Relationships
1. Check Your Ego:
Ego is a big turn off. Ego will end a relationship before you can really get it started. Serious misconceptions about chiropractors exist. Don’t play into that narrative. Throw ego into the mix and you’ve got no chance.
2. “Know Your Role”:
DCs are used to serving as the authoritarian figures in their offices. This mindset can lead to confrontation in the athletic training room or on the playing field. The ATC is the quarterback. The ATC organizes the huddle, calls the plays, audibles, distributes the ball and orchestrates the offense. The DCs role in many cases is that of the 3rd or 4th receiver. Picture a slot receiver who’s a key player on 3rd downs and in the red zone. DCs are often an invaluable member of the team but aren’t the star attraction. Get used to it. Know your role. Thrive in it. Serve the team to the best of your abilities.
3. The Magic is the Relationship:
Surround yourself with a great professional network and watch the magic happen. Sports med typically attracts a certain niche. The niche is type-A motivated professionals who work to be better, wish to serve, want to win and prefer success within a team setting. They want their athletes performing at peak level just as you do. You want to work in a dynamic setting like this. Nurturing relationships in this environment benefits all parties involved. It worked for us and it can work for you.
4. Relationships Take Work:
Even the best relationships take work. You don’t just do one nice thing a year for your spouse on their birthday or Christmas. You appreciate your spouse in small ways daily. Holding a door open for your wife isn’t a big thing, but it is appreciated and it does get noticed.
a. Lunches & Coffee Drops:
We did this once per semester (2x yearly). Coffee drops created better “top of mind” awareness.
b. In-services:
Teachers periodically have in-service days. Utilize this concept and create one in-service day per semester. Create a theme. Have each team member contribute an article, video or lead a practical session during the in service. We led an in-service on gait mechanics and orthotics, for example. We covered our gait exam, orthotic evaluation, and casting procedures.
c. Lecturing:
Ask the athletic trainers if they have a sports medicine, anatomy or physiology class. See if you can guest lecture during one of the classes on a topic of interest.
d. Career Day:
Ask to be a guest speaker at a career day. This is a great way to get a couple minutes of face time with the athletic trainers. Career day speaking spreads your brand in the community as well as inspires the next generation of chiropractors.
e. Shadowing:
One of the best ways to develop relationships is to shadow sports med team members on site, on their turf. It’s a slam dunk, cost-effective marketing strategy that builds trust. Shadow the orthopedist in their office. Shadowing on their turf shows a genuine passion to learn, grow and play as a team member.
f. Scheduling:
There’s a quote by Woody Allen that says “80% of success is just showing up.” Simply put, show up and maintain a positive attitude. Collaborate with the ATCs to come up with a schedule based on their needs. When is their busy time of year? What tournaments do they need help covering? What other obstacles are present that impact the ability to deliver sports medicine services? Make a schedule and stick to it as best as possible.
g. On Site Injury Checks:
I didn’t utilize this tool as much as I could have, to be honest, but colleagues such as a team orthopedists and other sports chiropractic colleagues utilized this tool to great success. Set aside sometime during the school week and perform free injury checks at the school. This saves the parent and athlete time and money for scheduling an in-office visit. What seemed to be effective without over-reaching was 2 days/month for one hour near the conclusion of practice.
For example, on-site injury checks were performed on the 1st and 3rd Thursdays of every month that school was in session. Make sure to coordinate with the athletic trainer to confirm his/her availability along with athlete availability. It’s also a great idea and wise from a medicolegal standpoint to have the parent (medical decision maker) present to grant consent and avoid student to parent miscommunication typical of teenagers. This is also a small window into the parent-athlete relationship, which could matter in the athlete’s outcome. Additionally, the parents are ultimately the ones “investing” in treatment. It helps to gauge parent interest so neither party wastes time and money.
h. Staff Dinners & Social Outings:
This was a fun activity that we started after trust was built. Typically, we went out for a sports med team social outing to a local gastro pub 2x/yearly. Often, it was after the last home Friday night football game and towards the end of the school year. The group outing may be used a business expense under certain conditions (review with your tax professional in light of recent tax amendments).
i. Professional Newsletter & Content:
Add the sports med staff to your professional newsletter and create custom content for them. What do they want to know about? What weaknesses do they have? What strengths can you share with them? What do they need to know about you or your practice to effectively help their athletes or their patients? We sent over a custom e-newsletter quarterly with relevant content.
j. Donation:
Schools, clubs and smaller organizations have limited budgets. Often the athletic trainers are given lemons and need to make lemonade. If there’s a need and you are able, step up and offer some financial assistance. We donated free orthotic foam casts for a sports medicine orthotic casting lab. It wasn’t a big investment, but it was appreciated because the casts were not approved in the sports med budget. It saved the awkward conversation of the athletic trainers asking mom or dad unexpectedly for $30 to purchase a one-time use foam cast for the student’s sports med course requirements.
5. Market Your Outcomes:
One of the central themes of sports medicine is a rapid, safe return to action. Many athletic trainers don’t know a subset of evidence-based, sports medicine trained, rehab minded DCs exist who are able to rapidly and safely return an athlete to competition. This is where you can change the narrative. Providing athletes with rapid recovery and outstanding outcomes by obtaining functional and measurable baselines will blow the ATC’s mind. Imagine taking an ankle sprain from crutches to return to prior levels of performance within 4-6 visits over a 2-3 week time period. Imagine that athlete demonstrating the ability to descend an 8-inch step down symmetrically R vs. L with good neuromusculoskeletal control.
Imagine that athlete showing the ATC or the team physician that the 6-8 week time frame for recovery was far too conservative. Imagine the athlete actually demonstrating the improved 8” step down test directly in front of the ATC or the orthopedic medical physician. Imagine that you stated this goal from the start and communicated progress with your sent notes. Imagine that you’ve data-tracked 50 or 100 ankle sprains in your athletes, looking at the outcomes assessments, number of visits, and other return to play criteria. Imagine you are leveraging that data to guide your opinion on a speedy recovery. Imagine you followed up with a phone call to the ATC and to the orthopedic medical physician after the initial assessment and at discharge. Imagine that you’ve created collateral marketing pieces around that data about your successful outcomes to distribute to the other team members and into the community. You’ve marketed yourself ethically and extremely well in this scenario. You’ve let your outcomes, data and communication do the talking. You will sound like someone with whom any rational sports med professional would want to do business.

6. This is a Marathon, Not a Sprint:
One of the most common faults is taking the relationship for granted or forgetting about it, once it is established. The strategy here is to maintain top of mind awareness. Don’t take the relationship for granted. Be present, but not overwhelming. The marketing strategy is to play the long game. Recognize this is a marathon, not a sprint.
7. Give So That You Can Receive:
Nothing greases the wheels of a referral relationship like giving. By placing your trust in another professional, you’ll earn his or her trust. This is especially true if the patient you are sending has positive reviews of your care, whether you helped them or not. The big point is that you were truthful, trustworthy and able to recognize strengths vs. limitations. You didn’t waste the patient’s resources of time, money and hope. Everyone appreciates. You’ve created a win-win scenario.
Conclusion
Don’t be deterred by the fact that the DC-ATC relationship can take some understanding and work! When handled with knowledge and sensitivity, it can be beneficial for you, the entire sports med team and the patient.
*** Disclaimer:
The views and opinions above represent that of the author, Dr. Dino Pappas. They do not reflect the official policy or position of any agency or company that Dr. Dino Pappas may have a relationship or affiliation with. ***

















