Managed Care Contracts

Managed Care Contracts: Read Before You Sign
Unfortunately, health insurance coverage for a patient is not a right in the United States. From a patient’s perspective, they desire coverage and they desire you, their doctor, to be in their Preferred Provider Organization (PPO) Network. As their treating doctor, or as a potential doctor in the network, you want to be there for the patient. Before signing any PPO or managed care contract, you have to make sure that your decision is a sound business decision.
I often will be sent an unsolicited proposal from a PPO network to be in their network. On other occasions, I may call and ask the insurance company to send me a contract, if one of my patients has a PPO that I am not in their network. Every doctor should keep in mind that you must read the contract first and decide if involvement in the PPO network is right for you.
Interestingly, I find that in some networks, I am actually reimbursed better if I am not in their network. It is advisable to review the fee schedules to assist you in deciding whether it is to your advantage to be in the network. It is advised that you carefully read any PPO contract before signing it. In many cases, you may wish to consult with an attorney for any legal ramifications in the contract.
Managed Care Contract provisions that may give you cause for further review:
- Chiropractic services limited only to the neuromusculoskeletal system. These may limit your role as a primary provider, which is allowed in the state of Illinois. Reimbursement for treatment is disallowed for conditions such as asthma, constipation or otitis media.
- Limitation of the number of visits a patient may be seen throughout the year or for a given condition, regardless of the need for care or progress in their condition.
- Reimbursement rates that require a PPO discount that is greatly below charges that are considered customary and reasonable for your locality.
- Provisions that do not pay for examinations or re-examinations.
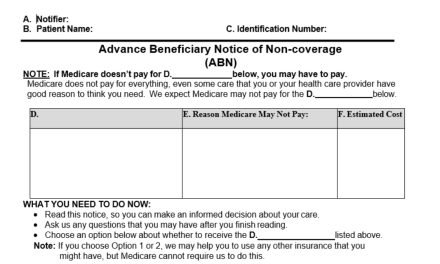
- Requirement to use only certain forms provided by the managed care organization, and that all others that you may utilize become null and void.
- Requirement by the managed care organization to allow inspection of any financial or administrative records of the doctor’s practice
- Provisions to require certain hours of operation of the office or of your office location.
- Provisions that require electronic billing, even if you do not use any type of electronic billing.
- Restriction as to the use of x-ray procedures.
- Restriction that prohibits you from using a legal service or collection agency for collection of delinquent patient accounts.
- Restrictions that prohibit you to bill the patient in any manner for services rendered.
- Agreement to provide medical records copies at no charge. Illinois law allows fees to be charged for the reproduction of records in most cases.
- A contract which restrains you in any way after the termination of the contract.
- A contract in which allows the company to release or sell your information to other PPO networks. Often, if you join one network, another network will automatically enroll you without your approval of their contract.
- Contracts that pay no benefits whatsoever to the chiropractor or to the patient. The patient pays the fee to the chiropractor minus the discount.
Summary
A managed care agreement is a binding contract between you and the insurance company. As with any legal document, the restrictions and provisions listed above should give you cause to carefully consider any contract before you sign. This body of work is not to be misconstrued as legal advice, but only to demonstrate the need for you to read the contract before you sign it and to engage appropriate legal counsel.