Congenital Hypoplasia of the Posterior Arch of the Atlas: Radiographic Findings and Clinical Considerations

A 65-year-old male with intermittent chronic neck pain presented to his chiropractic physician’s office. He had non-specific orthopedic exam findings and a normal neurologic exam. Patient denies any history of abnormal neurologic symptoms. Radiographic examination of the cervical spine reveals complete aplasia of the posterior arch of the atlas with hyperplasia of the C2 spinous process (Figure 1). Based on the normal neurologic exam findings and no reported neurologic symptoms, no further follow-up was required.

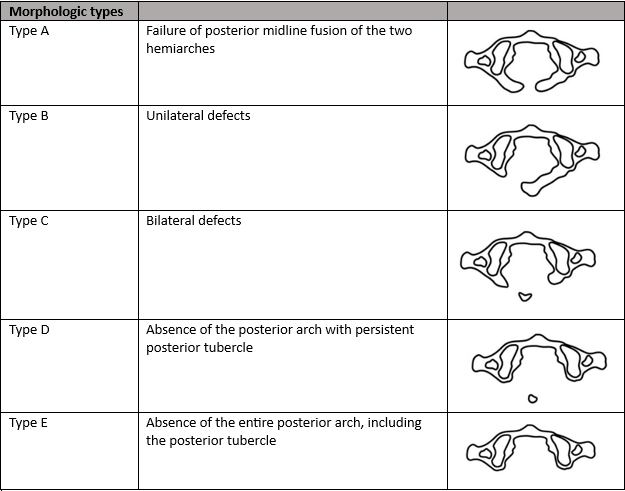
Hypoplasia of the posterior arch of the atlas is an uncommon congenital anomaly that is seen in up to 4% of the population.1. These anomalies are often considered simply benign congenital anomalies without clinical significance; however, this assumption is not always the case. The degree of posterior arch hypoplasia may range from a thin posterior midline defect, due failure of midline fusion of the two hemiarches, to complete aplasia of the posterior arch. Clinicians often find these defects incidentally on cervical spine radiographs but may be unsure of how to proceed after discovering the anomaly. This article will focus on understanding the different morphologic types of hypoplasia of the posterior arch of the atlas, as well as clinical considerations based on radiographic and clinical findings.
The most commonly used classification system is the Currarino classification, which describes both morphological types and clinical subgroups.2
Clinical subgroups Subgroup 1 Incidental imaging finding, asymptomatic Subgroup 2 Neck pain or stiffness after trauma to head or neck Subgroup 3 Chronic symptoms referrable to the neck Subgroup 4 Various chronic neurologic symptoms Subgroup 5 Acute neurological symptoms following minor cervical trauma
Isolated hypoplasia of the posterior arch of the atlas variations are generally considered benign anomalies and are generally asymptomatic; however, neurologic symptoms, ranging from mild neck pain to intermittent quadriparesis, have been found to occur with cervical extension or after minor cervical traumaquadriparesis.1,3 Type A and subgroup 1 are the most common and account for 80-90% of the cases.1 These cases do not seem to place the patient at neurologic risk. Type C and D are considered to potentially be problematic due to the possibility of impingement of the cord by the posterior tubercle during extension.
The transient nature of the neurologic symptoms or their appearance following minor cervical trauma appears to correlate with the anatomic observations associated with the Type C and D anomalies. It is suggested that in Types C and D (those with an isolated posterior bony fragment) that inward mobility of the posterior fragment is possible.4. Autopsy and surgical studies have shown that the gap between the osseous fragments is bridged by loose connective tissue, rather than cartilage. Therefore, it is possible that the isolated posterior tubercle can move in dissociation from the anterior arch. This is particularly important to consider during cervical extension in which cord impingement may occur due to a reduction in the distance between the occiput and the spinous process of C2, which can lead to inward buckling of the attached ligaments causing displacement of the isolated fragment anteriorly into the spinal canal.4 This compression of the cord can cause focal myelomalacia, cord edema, or a pre-syrinx state.4
When considering the appropriateness of cervical manipulation in patients with hypoplasia of the posterior arch of the atlas, it is important to consider each type separately. Please note that the term “cervical manipulation” will refer to high velocity low amplitude (HVLA) spinal manipulation and not soft tissue or low amplitude type manipulation. Neurologically stable patients with Type A or B do not appear to have the risk of cord impingement, and, therefore, manipulation would not be contraindicated. Type C and D (of any clinical subgroup) do have the risk of cord impingement during cervical extension and/or neurologic injury following minor trauma, and, therefore, in this author’s opinion, HVLA upper cervical manipulation and cervical extension-based soft tissue manipulation/ mobilization are contraindicated. Additionally, these patients should be advised to avoid contact sports, and advanced imaging studies (MRI unless contraindicated) should be performed in those patients that are neurologically symptomatic.4 Surgery is the treatment of choice in patients with instability or compression and may include posterior fusion or surgical excision of the posterior arch.
Our patient was a morphologic type E/ clinical subgroup type 1. The question was posed if this patient was at risk for neurologic sequelae with cervical manipulation. Review of the literature suggests that the risk of cord impingement is not a factor in the morphologic group E, but that instability may occur. Therefore, before any cervical manipulation is performed, cervical flexion and extension radiographs are needed to rule out upper cervical instability. Assuming the patient is neurologically asymptomatic (particularly in extension) and no instability is present, there is no literature to suggest that cervical manipulation is contraindicated. Treatment for patients with hypoplasia of the posterior arch of the atlas should be carefully examined, properly imaged, and treated in accordance with symptoms pre- and post-manipulation (if indicated).
References
- Sabuncuoglu H, Ozdogan S, Karadag D, Kaynak ET. Congenital hypoplasia of the posterior arch of the atlas: case report and extensive review of the literature. Turk Neurosurg. 2011 Jan;21(1):97-103. PMID: 21294100.
- Currarino G, Rollins N, Diehl JT. Congenital defects of the posterior arch of the atlas: a report of seven cases including an affected mother and son. AJNR Am J Neuroradiol. 1994 Feb;15(2):249-54. Erratum in: AJNR Am J Neuroradiol 1994 Jun;15(6):A9. PMID: 8192068; PMCID: PMC8334620.
- Torreman M, Verhagen IT, Sluzewski M, Kok AJ, van Rooij WJ. Recurrent transient quadriparesis after minor cervical trauma associated with bilateral partial agenesis of the posterior arch of the atlas. Case report. J Neurosurg. 1996 Apr;84(4):663-5. doi: 10.3171/jns.1996.84.4.0663. PMID: 8613860.
- Sharma A, Gaikwad SB, Deol PS, Mishra NK, Kale SS. Partial aplasia of the posterior arch of the atlas with an isolated posterior arch remnant: findings in three cases. AJNR Am J Neuroradiol. 2000 Jun-Jul;21(6):1167-71.