
Avoid Duplication of Diagnoses

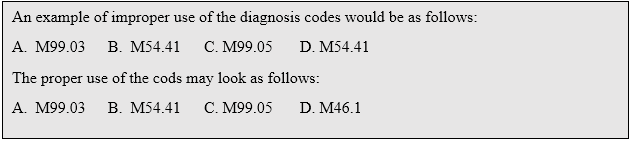
Although multiple segments or regions may be involved in the cause of a patient’s ailment, it is important to identify the main segment or region and report the diagnosis specifically. Medicare has recently reaffirmed that duplication of diagnoses in Box 21 on the claim form will be denied. Each area treated must have a unique diagnosis.
Effective July 2, 2018, CMS-1500 hard copy claims should not list the same ICD-10-CM diagnosis code twice within item 21. Medicare Administrative Contractors (MACs) and Durable Medical Equipment (DME) MACs have been instructed to return these claims as unprocessable.
Diagnosis Codes my be reported once per encounter
ICD-10 version 5010 instructions state, “Each unique ICD-10-CM diagnosis code may be reported only once per encounter. This also applies to bilateral conditions when there are no distinct codes identifying laterally or two different conditions classified to the same ICD-10-CM diagnosis code.”
Medicare has implemented system changes to ensure that all Part B 837 coordination of benefits/Medicare crossover claims do not include duplication of diagnosis codes. Claims with a diagnosis code listed more than once within item 21 on the claim form will be rejected, based on Claim Adjustment Reason Code (CARC) 16, Remittance Advice Remark Code (RARC) M76, and alert RARC N211.
In addition, guidance in the HIPAA Technical Report Guide governing 837 professional claims transactions says to use distinct diagnoses pointers to differentiate among multiple diagnosis codes. Although you do not use the same diagnosis in box 21 for different regions, it is required to only use the letter A in the diagnosis pointer 24J. Commercial carriers, such as Blue Cross, allow the use of multiple pointers in box 24J, but Medicare requires only the letter A in 24J.
In the past, Medicare’s Contractor Common Edits routinely caught situations where diagnosis code references are used more than once in box 21. As of July 2, 2018, there is now a reason code established to identify the reason for the rejection. In the past, claims with duplication of diagnosis were rejected and sent back with the error reported as “H54271 ICD-10 codes cannot be duplicated” through Medicare’s 277-CA process. This affects primarily incoming hard copy (CMS-1500) claims.
It is recommended that providers and their staff are aware of these enforcements. Policies and procedures should be altered as needed to conform to these regulations.



















