Achilles Injuries and Tendinopathy

Introduction & Etiology
The Achilles tendon is the largest and strongest tendon in the human body but is simultaneously a vulnerable link in the locomotion chain. (1) The tendons’ structural prowess is relentlessly confronted by functional demands that can be up to 12 ½ times body weight while running. (2)
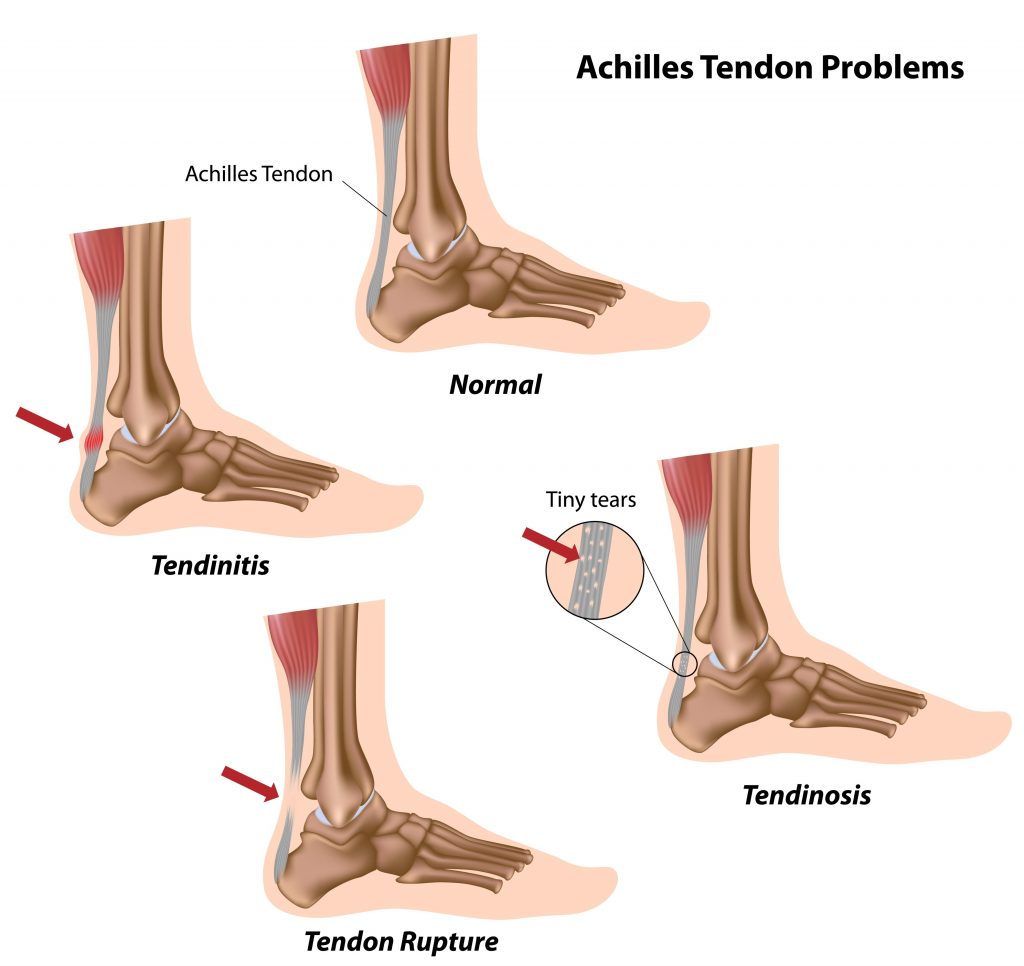
The Achilles tendon may be acutely strained or ruptured as the result of an excessive stretch or eccentric force. Consistent with other types of acute strains, Achilles tendon injuries may occur when the musculotendinous unit transitions from eccentric deceleration to concentric propulsion. This happens during the “mid-stance” phase of gait. (3) Strains occur when collagen fibers are stretched by more than 4%. Ruptures occur when stretch exceeds 8%. (4,5)
Tendinopathy
Unlike acute injuries that cause inflammation, tendinopathy is characterized by repeated overloading, micro-tearing, failed healing, and subsequent tendon degeneration. (3,4,6,7) The process begins with collagen fiber disruption and ends in a disorganized healing process that fails to regenerate a “normal” tendon. Failed healing is blamed on a hyperplastic, but ineffective, microvascular system. (8,9)
An appreciation of gait mechanics is germane to understanding Achilles tendon injuries. During normal gait, the foot approaches the ground with 3-4 degrees of supination, allowing ground contact to occur on the lateral portion of the calcaneus. As a shock-absorbing mechanism, the foot initially relaxes into subtalar pronation. At mid-stance, the foot converts into a rigid lever and begins to supinate in anticipation of propulsion. Tibial external rotation accompanies ankle supination. Inefficient conversion from shock absorber to rigid lever results in hyper pronation, which stresses the medial calcaneotendinous attachment of the Achilles tendon. (10)
Classifications of Injuries
Injuries to the Achilles tendon may be classified as “insertional” or “non-insertional.” Insertional tendinopathy, as its name implies, describes damage to tendon fibers at their insertion on the posterior calcaneus. This process may result in calcification and bony exostosis, producing a prominent enlargement of the posterior calcaneus, also called a “Haglund deformity” or “pump bump.” Non-insertional Achilles tendinitis most commonly involves the vulnerable “watershed area,” 2-6 cm proximal to the calcaneal insertion. (11) This region of the tendon has a smaller cross-sectional area, is relatively hypovascular, and is subject to a repetitive “wringing” motion during supination/ pronation. This susceptible mid-section is the most common site for degeneration and rupture. (12,13)
Achilles tendon injuries affect between 250,000 and 1 million people per year in the United States. (14,15) Most are middle-aged males in their third or fourth decade of life. (14,16) Interestingly, Achilles tendon injuries occur more frequently on the left side. (16) Injury rates are highest in the spring months and lowest in the fall. (93) Patients who have suffered prior Achilles tendon rupture are at significantly higher risk for contralateral tendon rupture. (17)
Athletes
Two-thirds of all Achilles tendon injuries involve athletes. (18) Runners are up to 10 times more likely to suffer Achilles tendon injuries, compared to age-matched controls. (18) The Achilles is the most common site of tendinopathy in runners. (77) Athletes are at greater risk during speed training or sprinting. (19) Runners who assume a midfoot or forefoot strike pattern may be at even greater risk of injury. (20) Not surprisingly, a higher risk has been identified in other sports that involve running or jumping. The estimated incidence of Achilles tendinopathy is: running sports, 53%; soccer, 11%; dance, 9%; gymnastics, 5%; racquet sports, 2%; football, 1%. (14,21)
Extrinsic risk factors for Achilles injury include improper warm-up, overtraining, cold-weather training, running on hard surfaces, excessive stair or hill climbing, improper arch support/ footwear, poor conditioning and abruptly returning to activity after a period of inactivity. (19,22-26,94) Wearing high-heeled shoes may lead to shortening of the gastrocnemius/soleus, predisposing women to Achilles tendinopathy. (27) Intrinsic factors include, prior lower limb fracture, hyper pronation, pes planus, cavus foot, gastrocnemius/soleus inflexibility or weakness, limited ankle dorsiflexion, and limited subtalar motion. (14,22-26,94,96) Systemic risk factors include diabetes, hypertension, inflammatory arthropathy, gout, obesity, and the use of corticosteroids or quinolones (broad-spectrum antibiotics). (28,81,84,94)
Clinical Presentation
Patients may present with symptoms from an acute strain or a more gradual onset of repetitive irritation. Complaints include pain or tenderness in the tendon or heel that intensifies with activity, especially walking or running. Patients may report difficulty when attempting to stand on their toes or walking steps, particularly down stairs. Morning pain and stiffness are common. Patients may report warmth and swelling that increases throughout the day, related to activity. Symptoms may be tracked using the VISA-A questionnaire. (29)
Palpating the point of maximum tenderness can help localize the site of injury to either the “watershed area,” or the calcaneal insertion. Mid tendon pain suggests non-insertional tendinitis, whereas posterior calcaneal pain suggests insertional tendinitis. Fusiform swelling and tendinous or bony enlargement are common in cases of chronic tendinopathy. Those with insertional tendinopathy may demonstrate evidence of bony enlargement or spurring on the posterior calcaneus.
Testing
Range of motion testing will likely reveal deficits in passive dorsiflexion, with pain on resisted plantar flexion. In some patients, single-leg heel raises will elicit pain, while in others, repetitive hopping may be needed to elicit complaints. The Silfverskiold test can help differentiate Achilles vs. gastrocnemius tightness in patients with limited dorsiflexion. Clinicians may perform the “calf squeeze test” (Thompson test) to exclude tendon rupture in those who have difficulty ambulating. The test has excellent validity and is performed by squeezing the calf of a prone patient and observing for passive plantar flexion of the foot. (30) Clinicians should perform motion palpation of the subtalar joint to assess mobility and identify restrictions.
Plantaris tendon pathology is associated with chronic mid-portion Achilles tendinopathy. (87-89) The plantaris tendon typically resides deep and adjacent to the Achilles medial border. Repetitive irritation of either tendon may lead to inflammation, scar tissue formation, and adhesion. This restricts gliding and leads to painful tethering when load is applied. (90) In some cases, the plantaris tendon has been known to thicken or even invaginate into the Achilles tendon, thereby thwarting traditional conservative management of Achilles tendinopathy. Tenderness on the medial mid-tendon is suggestive of plantaris involvement, while ultrasound or MRI may be necessary for a definitive diagnosis.
Assessing for Deficits
Clinicians must assess for contributory functional deficits throughout the kinetic chain. Runners with non-insertional tendinopathy demonstrate an increased incidence of foot hyperpronation (subtalar eversion). (76) Foot hyperpronation manifests as loss of the medial longitudinal arch, forefoot abduction (i.e. “too many toes sign”), calcaneal eversion, and navicular drop. Assess for weakness in the posterior tibialis by observing for calcaneal eversion during heel raises. Gastrocnemius/soleus flexibility may be assessed by measuring and comparing passive ankle dorsiflexion. Clinicians should assess knee flexor/hamstring strength, as weakness in this muscle is a known risk factor for Achilles tendon pain. (31) Weakness or delayed activation of the hip abductors (gluteus medius) should be identified and corrected. Functional orthopedic testing for hip abductor weakness would include the Trendelenberg sign, overhead squat test, and single-leg squat test. Weakness or delayed activation of the gluteus medius is associated with ankle dysfunction. (32)
Hallux limitus (limitation in passive dorsiflexion of the first metatarsophalangeal joint) disrupts normal foot functional stability and has been associated with Achilles tendon pain. (33) Functional hallux limitus assessment is performed on a long-sitting patient. The clinician places a thumb under the patient’s first metatarsal head and forces the patient’s foot into maximum dorsiflexion and pronation to simulate a ground reaction force. The clinician then pinches the patient’s great toe with their opposite hand and passively moves the toe into dorsiflexion. Dorsiflexion of the great toe should be fluid and produce concurrent plantar flexion of the patient’s metatarsal head into the clinician’s thumb. A sense of “jamming” or “locking” upon dorsiflexion or a lack of concurrent first metatarsal plantarflexion suggests hallux limitis. Assessment of the patient’s shoe insole may help to identify hallux limitus by revealing a lack of wear under the first metatarsal head with disproportionate wear under the second through fifth metatarsal heads and pad of the great toe. (34)
Diagnostics & Differential
Radiographs are often unnecessary for the diagnosis of Achilles tendinopathy. (35) The Ottowa Ankle Rules define the appropriateness for imaging patients with ankle or midfoot pain, following trauma. (36-38,74,75) No clearly defined rules exist for imaging non-traumatic heel pain. Clinicians may consider radiographs in cases of significant trauma with altered gait or when necessary to rule out other pathology, including calcaneal epiphysitis/avulsion. Radiographs of Achilles tendinopathy may demonstrate tendon calcifications and spurs/ enthesophytes on the posterior calcaneus. Ultrasound may be an efficient cost-effective means of evaluating the Achilles tendon. (39) Ultrasound or MRI may help identify and define tendon pathology.
The differential diagnosis for Achilles tendinopathy includes fracture, avulsion, neoplasm, infection, ankle sprain, retrocalcaneal bursitis, posterior ankle impingement, Os-trigonum syndrome, tenosynovitis, tendon dislocation, gastrocnemius musculotendinous strain (tennis leg), sural neuroma, systemic inflammatory disease, and calcaneal apophysitis (Sever’s disease). In children and adolescents, the epiphyseal growth plate is 2 to 5 times weaker than in adults. This group is more likely to suffer epiphyseal injuries in the form of calcaneal apophysitis (Sever’s disease) from stressors that would likely cause Achilles tendinopathy in adults. (40)
Management
Nonoperative treatment is the mainstay for Achilles tendinopathy. (81) “Traditional” treatment plans based solely on rest, therapy modalities, orthotics, and NSAIDs have failed to demonstrate benefit for Achilles tendinopathy patients. (41) Passive modalities including ice, ultrasound, electrical stimulation, and low-level laser also lack support. (42) The current standard of care for Achilles tendinopathy includes a combination of rest, eccentric rehabilitation, and correction of mechanical faults. Studies have demonstrated excellent results in up to 85% of patients undergoing appropriate conservative care. (43) Initially, patients may need to limit or stop activities that cause pain. Significant strains may require the use of crutches or a boot. Runners may need to switch to swimming, cycling, or other activities that limit stress to the Achilles tendon. Less stiff shoe soles will help to dissipate force and decrease Achilles strain when landing. (97) Patients should avoid shoes with an excessively rigid heel tab to reduce irritation.
Eccentric exercise programs are effective in treating Achilles tendinopathy. (41,44-54) Eccentric training is more effective than concentric training for reducing pain and improving function. (52,55) In fact, research suggests that eccentric strength training programs are more than twice as effective as concentric programs for the treatment of Achilles tendinopathy. (52) A proven program by Alfredson (45) incorporates single leg eccentric heel drops off the edge of a step. Heel drops should be performed with the knee both straight and bent, three sets of 15 repetitions, twice per day for 12 weeks. One study suggested that deficits are more prevalent in the soleus as compared to the gastric so rehab must include bent-knee exercises that target this muscle. (96) Heel drops should occur slowly on a 4-10 second count. (56) The patient should use the non-injured leg to return to the “heel up” start position, thereby avoiding concentric contractions. Moderate pain during this exercise is acceptable but if the pain is excessive, the patient should assist downward motion with the non-injured leg.
The goal of tendinopathy rehab is to carefully balance stimulating a controlled musculotendinous inflammatory response without causing greater injury or exacerbating symptoms. Rehab should begin with moderate effort and low repetitions. Response to tensile loading may be assessed by the patient’s change in night pain. Increases in night pain indicate the current rehab load is excessive. Progression advances when the patient tolerates a given level of tensile load. (92)
Manipulation
Soft tissue manipulation, stretching, and myofascial release techniques are necessary to promote flexibility of the calf muscles. Stretching of the calf muscles should be performed with the knee straight to address the gastrocnemius and with the knee bent to lengthen the soleus. Clinicians should consider the use of IASTM to release adhesions within the Achilles tendon. As an additional benefit, IASTM may accelerate healing, possibly via controlled microtrauma. (57,78-80) Manipulation may be necessary to eliminate restrictions in the kinetic chain, particularly within the ankle. (58) Clinicians may consider the use of a 7-15 mm heel lift (bilaterally) to minimize dorsiflexion stress. Arch supports or orthotics may be necessary to correct hyperpronation. (76) Patients with hallux limitus may benefit from wearing shoe inserts with a “cut out” beneath the first metatarsal head. (59)
The treatments described thus far are directed at a “contractile dysfunction” model. If the patient’s complaints are not resolving as intended, it is important to consider the Mechanical Diagnosis Therapy (MDT) concept of “derangement”. Many cases of “derangement” tendinopathy have responded to end-range plantar flexion, although a recent review of the literature provides no clinical trials of this concept. End range plantar flexion is performed on a regular basis, 10 repetitions every 2-3 hours. A clinical indicator that the patient may respond well to repetitive end-range movements is worsening of symptoms after dorsiflexion exercises.
Athletes should introduce new activities slowly and avoid increasing activity, particularly running, by more than 10% per week. Runners should begin on smooth, shock-absorbent surfaces and start out at a lower intensity and distance, first increasing distance, then pace. Athletes should avoid training on hard or unlevel surfaces, including hills.
Return-to-play criteria for Achilles tendon strains or ruptures include the “Triple 5”:
1. Ankle dorsiflexion is within 5 degrees of the uninjured side,
2. Calf circumference (measured 10 cm distal to the tibial tuberosity) is within 5 mm of the uninjured side, and
3. The patient is able to perform 5 sets of 25 single leg heel raises. (60)
Conclusion
Patients who fail a trial of conservative care should be referred, but proven alternatives are scarce. Medical co-management is of limited benefit. NSAIDs may relieve symptoms but have little long-term effect on outcome. (61,62) Cortisone injections are unproven for the treatment of Achilles tendinopathy and carry a possible increased risk of tendon rupture. (63,64) Extracorporeal shock-wave therapy (ESWT) or platelet-rich plasma (PRP) injections are controversial alternatives. (65-68) ESWT (originally developed as lithotripsy) is thought to break up calcific deposits and stimulate fibroblast activity to encourage healing and may be appropriate for Achilles tendinopathy. (81,82,91). PRP treatments consist of injecting platelet-rich plasma into a tendon to create a concentrated trigger of growth factors and chemoattractants for macrophages and fibroblasts, which gradually repair the damaged collagen. (69) Some clinicians suggest benefit from PRP injections, but others refute its usefulness for Achilles tendinopathy, (81,83) including at least one randomized clinical trial. (70)
Conservative care has shown to be as effective as surgery for long-term pain relief, ROM, function, tendon force, and quality of life in cases of chronic tendinopathy. (98) In the event of Achilles tendon rupture, several studies report at least equivalent results between surgical and conservative management. (59,71,72,85)
References
1. O’Brien, M. Functional anatomy and physiology of tendons (1992) Clinical Sports Medicine 11:505-20
2. Komi PV, Fukashiro S, Jarvinen M. Biomechanical loading of Achilles tendon during normal locomotion. Clin Sports Med 1992;11: 521–31.
3. Gibbon, W.W., Cooper, J.R., Radcliffe, G.S. (1999). Sonographic incidence of tendon microtears in athletes with chronic Achilles tendinosis. British Journal of Sports Medicine 33, 129–30.
4. Kvist M. Achilles tendon injuries in athletes. Sports Med 1994;18:173–201.
5. Leppilahti JOS, Karpakka J, et al. Overuse injuries of the Achilles tendon. Ann Chir Gynaecol 1991;80: 202–7.
6. Kader, D., Saxena, A, Movin, T, and Maffulli, N. (2002) Achilles tendinopathy: some aspects of basic science and clinical management. British Journal of Sports Medicine 36, 239-249.
7. Astrom M. On the nature and etiology of chronic achilles tendinopathy. PhD thesis, Lund University, Sweden, 1997.
8. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). J Bone & Jt. Surg 1999. 81-A(2):259-278.
9. Leadbetter WB. Cell-matrix response in tendon injury. Clin Sports Med 1992;11(3):568-569
10. Footlogics. Lower Limb Biomechanics www.footlogics.co/lower –limb-biomechanics.html. accessed 1/2/14
11. Wren TAL, Lindsey DP, Beaupré GS, Carter DR. Effects of creep and cyclic loading on the mechanical properties and failure of human Achilles tendons. Ann Biom Engineering. 2003;31:710–717.
12. Jacobs BA. Achilles Tendon Rupture. emedicine. medscape.com accessed 1/2/14
13. Chen, Tony M.; Rozen, Warren M.; Pan, Wei-ren; Ashton, Mark W.; Richardson, Martin D.; Taylor, G. Ian. (2009) The arterial anatomy of the Achilles tendon: Anatomical study and clinical implications Clinical Anatomy vol. 22 issue 3, 377–385.
14. Gebauer M, Beil FT, Beckmann J, Sárváry AM, Ueblacker P, Ruecker AH. et al. Mechanical evaluation of different techniques for Achilles tendon repair. Arch Orthop Trauma Surg. 2007;127:795–799.
15. Lauer, Harvey. American Sports Data, Inc. A Comprehensive Study of Sports Injuries in the U.S., 2003.
16. Suchak AA, Bostick G, Reid D, Blitz S, Jomha N. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot and Ankle International 2005;26(11):932-936.
17. Aroen A, Helgo D, Granlund OG, Bahr R. Scand J Med Sci Sports. 2004 Feb;14(1):30-3.
18. Rolf CMT. Etiology, histopathology, and outcome of surgery in achillodynia. Foot Ankle Int 1997;18: 565–9.
19. Clement, D.B., Taunton, J.E., Smart, G.W. (1984). Achilles tendinitis and peritendinitis: Etiology and treatment. American Journal of Sports Medicine 12, 179–84.
20. Almonroeder T, Willson JD, Kernozek TW. The effect of foot strike pattern on achilles tendon load during running. Ann Biomed Eng 2013 May 3.
21. Kvist M. Achilles tendon overuse injuries. PhD thesis, University of Turku, Finland, 1991.
22. Asplund CA, Best TM. Achilles tendon disorders. BMJ. Mar 12 2013;346:f1262.
23. Keene JS. Tendon injuries of the foot and ankle. In: DeLee JC, Drez D, eds. Orthopaedic Sports Medicine. Philadelphia, Pa: WB Saunders; 1994:1788-94.
24. Albers D, Hoke B. Techniques in Achilles tendon rehabilitation. Tech Foot Ankle Surg. 2003;2(3):208-19.
25. Saltzman C, Bonar S. Tendon problems of the foot and ankle. In: Lutter LD, Mizel MS, Pfeffer GB, eds. Orthopaedic Knowledge Update: Foot and Ankle. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 1994:236-73.
26. Albers D, Hoke B. Techniques in Achilles tendon rehabilitation. Tech Foot Ankle Surg. 2003;2(3):208-19.
27. Csapo, R., Maganaris, C.N., Seynnes, O.R., Narici, M.V. (2010) On Muscle, Tendon and High Heels. Journal of Experimental Biology 213 3582-2588.
28. van der Linden, Paul D.; Sturkenboom, Miriam C. J. M.; Herings, Ron M. C.; Leufkens, Hubert M. G.; Rowlands, Sam; Stricker, Bruno H. Ch. (2003) Increased Risk of Achilles Tendon Rupture With Quinolone Antibacterial Use, Especially in Elderly Patients Taking Oral Corticosteroids JAMA Internal Medicine vol 163 no.15.
29. Robinson JM,Cook JL,Purdam C,Visentini PJ,Ross J,Maffulli N,Taunton JE,Khan KM;Victorian Institute Of Sport Tendon Study Group. Br J Sports Med. 2001 Oct;35(5):335-41.
30. Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med 1998. 26266–270.270.
31. Hein T, Janssen P, Wagner-Fritz U, et al. Prospective analysis of intrinsic and extrinsic risk factors on the development of Achilles tendon pain in runners. Scand J Med Sci Sports 2013 October 31
32. Nadler SF, Malanga GA, DePrince M, et al. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med 2000;10(2):89-97.
33. Payne C, Chuter V, Miller K. Sensitivity and specificity of the functional hallux limitus test to predict foot function. J Am Podiatr Med Assoc 2002;92(5):269-271.
34. Van Gheluwe B, Dananberg HJ, Hagman F, Vanstaen K. Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J Am Podiatr Med Assoc 2006;96(5):428-436.
35. Campbell R S D, Grainger A J. Current concepts in imaging in tendinopathy. Clin Radiol 2001. 56253–267.267.
36. Stiell IG, McKnight RD, Greenberg GH, McDowell I, Nair RC, Wells GA, Johns C, Worthington JR. Implementation of the Ottawa Ankle Rules. Journal of the American Medical Association 1994; 271:827-832.
37. Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Reardon M, Stewart JP, Maloney J. Decision Rules for the Use of Radiography in Acute Ankle Injuries.Journal of the American Medical Association 1993; 269:1127-1132.
38. Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Worthington JR. A Study to Develop Clinical Decision Rules for the Use of Radiography in Acute Ankle Injuries. Annals of Emergency Medicine 1992; 21:384-390.
39. Movin T, Gad A, Reinholt FP. Tendon pathology in long-standing Achillodynia. Biopsy findings in 40 patients. Acta Orthop Scand 1997;68:170–5.
40. Schwab SA. Epiphyseal injuries in the growing athlete. Can Med Assoc J 1977;117 : 626-630
41. Alfredson, H., Pietila, T., Jonsson, P., Lorentzon, R. (1998). Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. American Journal of Sports Medicine 26, 360–66.
42. Andres, Brett M.; Murrell, George A. C. (2008) Treatment of Tendinopathy: What Works, What Does Not, and What is on the Horizon Clinical Orthopaedics and Related Research 466(7)1539–1554
43. Anderson, D.L., Taunton, J.E., Davidson, R.G. (1992). Surgical management of chronic Achilles tendinitis. Clinical Journal of Sport Medicine 2, 38–42
44. Silbernagel KG, Thomee R, Thomee P, Karlsson J. Eccentric overload training for patients with chronic Achilles tendon pain‐‐a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports. Aug 2001;11(4):197‐206.
45. Maffulli N, Walley G, Sayana MK, Longo UG, Denaro V. Eccentric calf muscle training in athletic patients with Achilles tendinopathy. Disabil Rehabil. 2008;30(20‐22):1677‐1684.
46. Allison GT, Purdam C. Eccentric loading for Achilles tendinopathy‐‐strengthening or stretching? Br J Sports Med. Apr 2009;43(4):276‐279.
47. Fahlstrom M, Jonsson P, Lorentzon R, Alfredson H. Chronic Achilles tendon pain treated with eccentric calf‐muscle training. Knee Surg Sports Traumatol Arthrosc. Sep 2003;11(5):327‐333.
48. Jonsson P, Wahlstrom P, Ohberg L, Alfredson H. Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc. Jan 2006;14(1):76‐81.
49. Josza L, Kannus P. Human Tendons. Champaign, IL: Human Kinetics; 1997.
50. Knobloch K, Schreibmueller L, Kraemer R, Jagodzinski M, Vogt PM, Redeker J. Gender and eccentric training in Achilles mid‐portion tendinopathy. Knee Surg Sports Traumatol Arthrosc. May 2010;18(5):648‐655.
51. Maffulli N, Khan KM, Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy. Nov‐Dec 1998;14(8):840‐843.
52. Mafi N, Lorentzon R, Alfredson H. Superior short‐term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc. 2001;9(1):42‐47.
53. Sayana MK, Maffulli N. Eccentric calf muscle training in non‐athletic patients with Achilles tendinopathy. J Sci Med Sport. Feb 2007;10(1):52‐58.
54. Adel Shalabi, A., Kristoffersen-Wilberg, Svensson, L., Aspelin, P., and Movin, T. Eccentric Training of the Gastrocnemius-Soleus Complex in Chronic Achilles Tendinopathy Results in Decreased Tendon Volume and Intratendinous Signal as Evaluated by MRI. American Journal of Sports Medicine (2004)
55. Yu, JaeHo; Park, DaeSung; Lee, GyuChang . Effect of eccentric strengthening on pain, muscle strength, endurance, and functional fitness factors in male patients with achilles tendinopathy. Am J Phys Med Rehabil. 2013 Jan;92(1):68-76.
56. Khan KM, Cook JL, Taunton JE, Bonar F. Overuse tendinosis, not tendinopathy part 1: a new paradigm for a difficult clinical problem. Phys Sportsmed. May 2000; 28(5):38‐48.
57. Melham TJ, Sevier TL, Malnofski MJ, Wilson JK, Helfst RH. Chronic ankle pain and fibrosis successfully treated with a new non-invasive augmented soft tissue secondary to a history of repetitive use or excessive overload.
58. Dananberg, HJ, Shearstone, J, Guiliano, M “Manipulation Method for the Treatment of Ankle Equinus, “Journal of the American Podiatric Medical Association, 90:8 September, 2000 pp 385-389
59. Kilmartin TE, Wallace WA, Hill TW. Orthotic effect on metatarsophalangeal joint extension. J Am Podiatr Med Assoc 1991;81(8):414-417.
60. Saxena A, Ewen B, Maffulli N. Rehabilitation of the operated Achilles tendon: parameters for predicting return to activity. J Foot Ankle Surg 2011;50(1):37-40.tt61.
62. Almekinders L, Temple J. Etiology, diagnosis, and treatment of tendonitis: an analysis of the literature. Med Sci Sports Exerc 1998. 301183–1190.1190
63. Ryan, A.J. (1978). Injections for tendon injuries: Cure or cause. Physician and Sportsmedicine 6 (September), 39.
64. Shrier, I., Matheson, G.O., Kohl, H.W. (1996). Achilles tendonitis: Are corticosteroid injections useful or harmful? Clinical Journal of Sports Medicine 6, 245–50.
65. Alfredson H, Ohberg L. Sclerosing injections to areas of neo-vascularisation reduce pain in chronic achilles tendinopathy: A double-blind randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):338–44.
66. Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo achillis: A randomized controlled trial. Am J Sports Med. 2007;35(3):374–83
67. Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br. 2009;91(8):987–96.
68. Hawley JA. Handbook of Sports Medicine and Science, Running.
Blackwell Science (2008) ISBN:9780470756874
69. Monto RR. Platelet rich plasma treatment for chronic Achilles tendinosis. Foot Ankle Int. 2012 May;33(5):379-85.
70. Schepull, Thorsten; Kvist, Joanna; Norrman, Hanna; Trinks, Marie; Berlin, Gösta; Aspenberg, Per (2011) Autologous Platelets Have No Effect on the Healing of Human Achilles Tendon Ruptures – A Randomized Single-Blind Study. American Journal of Sports Medicine vol. 39 no. 1 38-47
71. Nilsson-Helander K, et al. Acute Achilles Tendon Rupture: A Randomized, Controlled Study Comparing Surgical and Nonsurgical Treatments Using Validated Outcome Measures Am J Sports Med August 27, 2010
72. Weber, Martin; Niemann, Marco; Lanz, Renate; Müller, Thorsten (2003) Nonoperative Treatment of Acute Rupture of the Achilles Tendon – Results of a New Protocol and Comparison with Operative Treatment. The American Journal of Sports Medicine Sept. vol. 31 no. 5 685-691
73. Soroceanu A, Sidhw F, Aarabi S, Kaufman A, Glazebrook M, Surgical Versus Nonsurgical Treatment of Acute Achilles Tendon Rupture: A Meta-Analysis of Randomized Trials JBJS Vol 94 Issue 23
74. Stiell I, Wells G, Laupacis A, Brison R, Verbeek R, Vandemheen K, Naylor D. A multicentre trial to introduce clinical decision rules for the use of radiography in acute ankle injuries. British Medical Journal 1995; 311:594-597.
75. Anis AH, Stiell IG, Steward DF, Laupacis A. Cost-effectiveness analysis of the Ottawa Ankle Rules. Annals of Emergency Medicine 1995; 26:422-428.
76. Ryan M,Grau S,Krauss I,Maiwald C,Taunton J,Horstmann T. Kinematic analysis of runners with achilles mid-portion tendinopathy. Foot Ankle Int. 2009 Dec;30(12):1190-5
77. Knobloch K,Yoon U, Vogt PM Acute and overuse injuries correlated to hours of training in master running athletes Foot & Ankle International. / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society2008, 29(7):671-676.
78. Davidson CJ, Ganion LR, Gehlsen GM, Verhoestra B, Roepke JE, Sevier TL. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 1997;29:313-319
79. Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31:531- 535.
80. Loghmani MT, Warden S. Instrument-Assisted Cross-Fiber Massage Accelerates Knee Ligament Healing Orthop Sports Phys Ther 2009;39(7):506-514.
81. Uquillas CA, Guss MS, Ryan DJ, et al. Everything Achilles: Knowledge Update and Current Concepts in Management. J Bone Joint Surg Am. 2015;97:1187-95
82. Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness
of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic
review. Am J Sports Med. 2015 Mar;43(3):752-61.
83. Maffulli N, Papalia R, D’Adamio S, Diaz Balzani L, Denaro V. Pharmacological
interventions for the treatment of Achilles tendinopathy: a systematic review of
randomized controlled trials. Br Med Bull. 2015 Mar;113(1):101-15. Epub 2015
Jan 12.
84. Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J
Sports Med. 2002 Mar-Apr;30(2):287-305.
85. Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Siira P, Laine V, Leppilahti J. A Prospective Randomized Trial Comparing Surgical and Nonsurgical Treatments of Acute Achilles Tendon Ruptures. Am J Sports Med. 2016 Sep;44(9):2406-14.
86. Spang C, Alfredson H, Docking SI, Masci L, Anderson G. The Plantaris Tendon. A Narrative Review Focusing On Anatomical Features And Clinical Importance. Bone Joint J 2016;98-B:1312–19.
87. Steenstra F, van Dijk CN. Achilles tendoscopy. Foot Ankle Clin 2006;11:429–438, viii.
88. Alfredson H. Midportion Achilles tendinosis and the plantaris tendon. Br J Sports Med 2011;45:1023–1025.
89. Calder JD, Freeman R, Pollock N. Plantaris excision in the treatment of non-inser-
tional Achilles tendinopathy in elite athletes. Br J Sports Med 2015;49:1532–1534.
90. van Sterkenburg MN, van Dijk CN. Mid-portion Achilles tendinopathy: why pain-
ful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc 2011;19:1367–1375.
91. Dedes V, Stergioulas A, Kipreos G, Dede AM, Mitseas A, Panoutsopoulos GI. Effectiveness and Safety of Shockwave Therapy in Tendinopathies. Mater Sociomed. 2018 Jun;30(2):131-146. doi: 10.5455/msm.2018.30.141-146.
92. Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2014;48:506-509.
93. Caldwell JE, Lightsey HM, Trofa DP, Swindell HW, Greisberg JK, Vosseller JT. Seasonal Variation of Achilles Tendon Injury. J Am Acad Orthop Surg Glob Res Rev. 2018;2(8):e043. Published 2018 Aug 22. doi:10.5435/JAAOSGlobal-D-18-00043
94. van der Vlist AC, Breda SJ, Oei EHG, Verhaar JAN, de Vos RJ. Clinical risk factors for Achilles tendinopathy: a systematic review. Br J Sports Med. 2019 Feb 4. pii: bjsports-2018-099991. doi: 10.1136/bjsports-2018-099991. [Epub ahead of print] Review. PubMed PMID: 30718234.
95. Yang J, Hodax JD, Machan JT, et al. Factors Affecting Return to Play After Primary Achilles Tendon Tear: A Cohort of NFL Players. Orthop J Sports Med. 2019;7(3):2325967119830139. Published 2019 Mar 12. doi:10.1177/2325967119830139
96. O’Neill S et al. Plantarflexor strength and endurance deficits associated with mid-portion Achilles tendinopathy: The role of soleus. Phys Ther Sport. 2019 Mar 9;37:69-76. doi: 10.1016/j.ptsp.2019.03.002. [Epub ahead of print]
97. Firminger CR et al. Effect of Shoe and Surface Stiffness on Lower Limb Tendon Strain in Jumping. Med Sci Sports Exerc. 2019 Apr 8.
98. Challoumas D, Clifford C, Kirwan P, Millar NL. How does surgery compare to sham surgery or physiotherapy as a treatment for tendinopathy? A systematic review of randomised trials. BMJ Open Sport Exerc Med. 2019;5(1):e000528. Published 2019 Apr 24.