Dysfunctional Breathing

Could Dysfunctional Breathing Be Suffocating Your Outcomes?
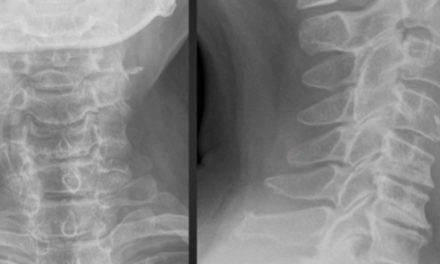
The diaphragm is necessary not only for respiration but for core stability as well. (1-3) The diaphragm is a key trunk stabilizer during postural activity and must properly activate upon demand. Dysfunctional breathing patterns may perpetuate many common musculoskeletal problems involving the head, neck, shoulder, and lower back. (4) Rehabilitation of dysfunctional breathing patterns is essential, yet often overlooked.

Intra-abdominal pressure (IAP) is a key determinant of core stability. (7-13) IAP is largely determined by the strength and tone of the muscles forming the “abdominal canister.” The front and sides of the abdominal canister are formed by the transverse abdominous and intercostal muscles. The back of the canister includes the paraspinal muscles, from the superficial spinal erectors to the deeper multifidi. The bottom of the canister is formed by the pelvic floor, while the diaphragm serves as the roof. Together, these muscles regulate intra-abdominal pressure and core stability. (14-24)
IAP
The stabilizing effect of IAP requires a complex synergy between all “canister” components. (25) The process begins when the diaphragm contracts to compress the abdominal cavity while the pelvic floor harmoniously co-activates to provide additional pressure. This is immediately followed by an eccentric contraction of the abdominal wall and lumbar extensor muscles, thereby maximizing intra-abdominal pressure and enhancing core stability. (25,26)
Trunk bracing protects the spine in a neutral position throughout movement. (26) A well-braced core also provides a stable foundation for extremity or head movement in much the same way that, when firing a cannon, a large ship serves as a better platform than a rowboat. In addition to healthy & functioning muscles, “stability” requires adequate central nervous system control. (5) The CNS must be able to reflexively brace the trunk in anticipation of movement. (28-32)
The Diaphragm
The diaphragm is the key modulator of intra-abdominal pressure. (33-37) The diaphragm must initiate pressurization by contracting before the abdominal wall. However, demands for increased stability (i.e. limb movement) do not always coincide with the initiation of a respiratory cycle. Fortunately, the diaphragm can adapt to perform its dual role of respiration and stabilization simultaneously. (36) The diaphragm’s postural contributions occur independently of breathing and may be controlled voluntarily, irrespective of the phase of respiration. (39,40) EMG studies demonstrate that the diaphragm contracts in anticipation of activity, irrespective of its respiratory phase. (40)
The body is generally able to co-manage its task of respiration during isolated brief limb movements. However, sustained or repetitive movements pose a challenge for the CNS. (40) The diaphragm’s role as a stabilizer varies greatly between individuals. (41) Patients who are unable to efficiently contract their diaphragm for postural stability have an increased risk of lower back pain and spinal disorders, including strain, disc lesion, and spondylolisthesis. (42-46)
“Normal” breathing occurs when the diaphragm contracts and flattens, pressurizing the abdomen and causing it to expand. The upper chest should remain relatively still. Patients with dysfunctional patterns often present with a “paradoxical” pattern where the abdomen remains still or retracts while the upper chest elevates and expands.
Diagnosis
The assessment of dysfunctional breathing begins with unannounced observation. Clinicians should look for classic signs of dysfunction including elevation of the upper rib cage, inadequate or asymmetrical lateral rib cage expansion, nasal flaring, labored breathing, frequent yawning, hyperventilation, mouth breathing, excessive paraspinal muscle contraction, and/or initiation of breathing from the chest rather than the abdomen. (49) The latter may be assessed with the patient lying supine, knees bent having the patient place one hand over their umbilicus, the other hand on their sternum. Initiation of a deep breath should start in the abdomen with minimal chest elevation. Normal breathing should cause a wave-like pattern of spinal flexion beginning at the diaphragm, then moving cephalad (best observed in a prone patient).
Detection of rib cage movement may be enhanced when the clinician stands behind the patient and places the (clinician’s) thumbs on the thoracolumbar paraspinal muscles with the second and third fingers lightly positioned over the patient’s lower ribs, while the fourth and fifth fingers are placed on the abdominal wall. As the patient breathes in and out, the clinician may monitor thoracolumbar paraspinal muscle contraction, rib movement, and abdominal wall resistance.
Clinicians may further assess the postural function of the diaphragm by placing their hands at the ends of the supine patient’s abdominal wall and instructing the patient to pressurize the abdomen while holding his or her breath. The clinician should feel pressure against both hands as the patient bears down. (41) Next, the clinician assesses for the preservation of abdominal pressure throughout the normal respiratory cycle by instructing the patient to maintain pressure while breathing. Finally, breathing & IAP should be assessed while the patient performs a functional movement like an overhead squat. (4)
Symptoms
Patients with dysfunctional breathing may rely on the accessory muscles of breathing. Myofascial irritation may be found in the: upper trapezius, scalenes, levator scapulae, SCM and/ or pectoral muscles. (4) Management should include assessment and correction of thoracic and costovertebral joint restrictions.
Treatment
Rehabilitation of dysfunctional breathing is an essential yet overlooked element of many treatment plans. In patients with “core problems,” diaphragmatic function should be restored prior to initiating balance or stability exercises. Patients with inadequate diaphragmatic function and poor stabilization may not benefit significantly from performing other core exercises. (50-54) Some authors believe that rehabbing abdominal and lumbar musculature prior to restoring diaphragmatic function may even “promote pathological patterns of movement and exacerbate the patient’s pain.” (50,52)
An article by Distano (4) provides an excellent progression for retraining proper breathing mechanics. Begin by educating the patient about the detrimental effect of abnormal breathing and how poor mechanics contribute to their symptoms. Briefly describe the patient’s abnormal breathing pattern and allow the patient to recognize his or her fault by manually palpating the areas of dysfunction breathing while observing themselves breath in a mirror. The clinician should demonstrate normal breathing mechanics, so that the patient may visualize proper abdominal and lower rib cage expansion while the chest remains still.
Clinicians should monitor the patient’s breathing rhythm to ensure that it is an ideal 1:2 ratio for inhalation and exhalation respectively. The ideal breathing cycle is three seconds of inhalation followed by six seconds of exhalation. Patients may be instructed to breathe in normally and then exhale through pursed lips in order to gradually increase the length of exhalation.
Training Proper Breathing Techniques
Training proper breathing techniques may begin with the patient in a supine hook-lying position, placing one hand on the abdomen and the other over the sternum. The patient should breathe in slowly and deeply through their nose. If the patient is breathing properly from the diaphragm, only the hand over the abdomen should rise, and the hand over the chest should remain still. Clinicians must stress the emphasis on abdominal expansion. Instruct the patient to lightly compress the abdomen while breathing in, followed by relaxation of the pressure while breathing out. The patient may apply light pressure to the lower lateral rib borders while inhaling and exhaling. The patient should practice two to three breaths hourly and 10-20 breaths upon awakening and retiring. Patients should “groove” proper breathing mechanics by practicing in a progressive fashion: first in a supine position, then seated, then standing, and finally, while performing dynamic movements (i.e. overhead squat).
Once the diaphragm is properly activating, rehab may progress to include other stability exercises. The ultimate goal of any spinal stability program is to re-train the CNS through repetitive exercise, to subconsciously maintain optimal centration and mechanics throughout activities of daily living, thereby reducing the risk of injury and improving performance. (56) Restoring spinal stability requires re-establishing a balanced co-activation of the diaphragm, pelvic floor, abdominals, and spinal extensors. Well-developed stability programs may decrease pain and improve trunk muscle function. (57-61) Specific exercises could include abdominal bracing exercises, planks, bird dog, and dead bugs. (41)
References
1. Hemborg B, Moritz U, Lowing H. Intra-abdominal pressure and trunk muscle activity during lifting. IV. The causal factors of the intraabdominal pressure rise. Scand J Rehabil Med. 1985;17:25-38.
2. Hodges PW, Butler JE, McKenzie DK, Gandevia SC. Contraction of the human diaphragm during rapid postural adjustments. J Physiol. 1997;505 pt 2:539-548.
3. Hodges PW, Richardson CA. Relationship between limb movement speed and associated contraction of the trunk muscles. Ergonomics. 1997;40:1220-1230.
4. Distano A, Evaluation and Management of Breathing Pattern Dysfunction in Spine Rehabilitation. http://www.ccptr.org/articles/peer-reviewed/evaluation-and-management-of-breathing-pattern-dysfunction-in-spine-rehabilitation/. Accessed 2/22/15.
5. Novotny, J.E., Beynnon, B.D., Nichols, C.E., 2000. Modeling the stability of the human glenohumeral joint during external rotation. J. Biomech. 33, 345e354.
6. Kolar P: Facilitation of Agonist-Antagonist Coactivation by Reflex Stimulation Methods In: Craig Liebenson: Rehabilitation of the Spine – A Practitioner’s Manual. Lippincott Williams & Wilkins, 2nd edition 2006, 531-565.
7. Cholewicki J, Juluru K, McGill SM. Intra-abdominal pressure mechanism for stabilizing the lumbar spine. J. Biomech. 1999a;32(1):13–17.
8. Cholewicki J, Juluru K, Radebold A, Panjabi MM, McGill SM. Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur Spine J. 1999;8(5): 388-395.
9. Cresswell AG, Grundström H, Thorstensson A. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiol. Scand. 1992;144(4):409–18.
10. Gardner-Morse MG, Stokes IAF. The effects of abdominal muscle co-activation on lumbar spine stability. Spine. 1998;23(1):86–92.
11. Hodges PW, Eriksson AE, Shirley D, et al. Intraabdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38(9):1873-80.
12. Hodges PW, Gandevia SC. Changes in intraabdominal pressure during postural and respiratory activation of the human diaphragm. J Appl Physiol 2000;89(3):967–976.
13. Shirley D, Hodges PW, Eriksson Ae, Gandevia SC. Spinal stiffness changes throughout the respiratory cycle. J Appl Physiol. 2003;95:1467-1475.
14. Cholewicki J, Juluru K, McGill SM. Intra-abdominal pressure mechanism for stabilizing the lumbar spine. J. Biomech. 1999a;32(1):13–17.
15. Cresswell AG, Grundström H, Thorstensson A. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiol. Scand. 1992;144(4):409–18.
16. Gardner-Morse MG, Stokes IAF. The effects of abdominal muscle co-activation on lumbar spine stability. Spine. 1998;23(1):86–92.
17. Hodges PW, Gandevia SC. Changes in intraabdominal pressure during postural and respiratory activation of the human diaphragm. J Appl Physiol 2000;89(3):967–976.
18. Shirley D, Hodges PW, Eriksson Ae, Gandevia SC. Spinal stiffness changes throughout the respiratory cycle. J Appl Physiol. 2003;95:1467-1475.
19. Hodges PW, Cresswell AG, Daggfeldt K, Thorstensson A. In vivo measurement of the effect of intraabdominal pressure on the human spine. J Biomech. 2001;34:347–353.
20. Hodges P, Kaigle-Holm A, Holm S, Ekström L, Cresswell A, Hansson T, Thorstensson A.
Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine. 2003;28(23):2594–601.
21. Kavcic N, Grenier S, McGill SM. Determining the stabilizing role of individual torso muscles during rehabilitation exercises. Spine. 2004; 29(11):1254–65.
22. Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001;537(Pt 3): 999-1008.
23. Gandevia SC, Butler JE, Hodges PW, et al. Balancing acts: respiratory sensations, motor control, and human posture. Clin Exp Pharmacol Physiol. 2002;29(1-2):118-21.
24. McGill SM, Grenier S, Kavcic N, Cholewicki J. Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol. 2003;13(4):353-359.
25. Kolar P, Neuwirth J, Sanda J, Suchanek V, Svata Z, Pivec M. Analysis of diaphragm movement during tidal breathing and during its activation while breath holding using MRI synchronized with spirometry. Physiol Res 58:383-392, 2009
26. Kolar P Postural Function of the Diaphragm in Persons With and Without Chronic Low Back Pain J Orthop Sports Phys Ther 2012;42(4):352-362, Epub 21 December 2011.
27. Kolar P, Sulc J, Kyncl M, Sanda J, Cakrt O, Andel R, Kumagai K, Kobesova A. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352-62.
28. Aruin AS, Latash ML. Directional specificity of postural muscles in feed-forward postural reactions during fast voluntary arm movements. Exp Brain Res. 1995;103:323-332.
29. Hodges P. Lumbopelvic stability: a functional model of biomechanics and motor control. In: Richardson C, Hodges P, Hides J, eds. Therapeutic Exercise for Lumbopelvic Stabilization. 2nd ed. Sydney, Australia: Churchill Livingstone; 2004:13-28.
30. Hodges PW, Cresswell AG, Daggfeldt K, Thor- stensson A. Three dimensional preparatory trunk motion precedes asymmetrical upper limb movement. Gait Posture. 2000;11:92-101.
31. Hodges PW, Richardson CA. Relationship between limb movement speed and associated contraction of the trunk muscles. Ergonomics. 1997;40:1220-1230. http://dx.doi. org/10.1080/001401397187469
32. Hodges, P. W., Butler, J. E., McKenzie, D. & Gandevia, S. C. (1997). Contraction of the human diaphragm during postural adjustments. Journal of Physiology 505, 539—548.
33. De Troyer A, Loring SH. Action of the respiratory muscles. In: Macklem PT, Mead J, eds. Handbook of Physiology: Section 3: The Respiratory System Volume III, Parts 1 & 2: Mechanics of Breathing. New York, NY: Oxford University Press; 1986:443-462.
34. Hodges PW, Cresswell AG, Daggfeldt K, Thor- stensson A. In vivo measurement of the effect of intra-abdominal pressure on the human spine. J Biomech. 2001;34:347-353.
35. Hodges PW, Eriksson AE, Shirley D, Gande- via SC. Intra-abdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38:1873-1880. http://dx.doi.org/10.1016/ J. Biomech.2004.08.016
36. Kolar P, Sulc J, Kyncl M, et al. Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment. J Appl Physiol. 2010;109:1064-1071. http://dx.doi. org/10.1152/japplphysiol.01216.2009
37. Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5:383-389; discussion 397.
39. Kolar P, Neuwirth J, Sanda J, Suchanek V, Svata Z, Pivec M. Analysis of diaphragm movement during tidal breathing and during its activation while breath holding using MRI synchronized with spirometry. Physiol Res 58:383-392, 2009
40. Zedka, M. & Prochazka, A. (1997). Phasic activity in the human erector spinae during repetitive hand movements. Journal of Physiology 504, 727—734.
41. Reinold M. Core Stability From the Inside Out. www.mikereinold.com Accessed 2/22/15
42. Cresswell AG, Oddsson L, Thorstensson A. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing. Exp Brain Res. 1994;98:336-341.
43. Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976). 1994;19:165-172.
44. Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80:1005-1012.
45. Kalpakcioglu B, Altinbilek T, Senel K. Determination of spondylolisthesis in low back pain by clinical evaluation. J Back Musculoskelet Reha- bil. 2009;22:27-32. http://dx.doi.org/10.3233/ BMR-2009-0212
46. Kolar P, Sulc J, Kyncl M, Sanda J, Cakrt O, Andel R, Kumagai K, Kobesova A. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352-62.
47. Janssens L, Brumagne S, Polspoel K, Troosters T, McConnell A. The effect of inspiratory muscles fatigue on postural control in people with and without recurrent low back pain. Spine (Phila Pa 1976). 2010;35:1088-1094.
48. O’Sullivan PB, Beales DJ, Beetham JA, et al. Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. Spine (Phila Pa 1976). 2002;27: E1-8.
49. Kolar P, Sulc J, Kyncl M, Sanda J, Cakrt O, Andel R, Kumagai K, Kobesova A. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352-62.
50. Kobesova A, Kolar P. Developmental kinesiology: Three levels of motor control in the assessment and treatment of the motor system. Journal of bodywork and movement therapies 01/2014; 18(1):23-33.
51. Akuthota, V., Ferreiro, A., Moore, T., Fredericson, M., 2008. Core stability exercise principles. Curr. Sports Med. Rep. 7, 39e44. http://dx.doi.org/10.1097/01.
52. Kobesova, A., Kolar, P., Mlckova, J., Svehlik, M., Morris, C.E., Frank, C., Lepsikova, M., Kozak, J., 2012. Effect of functional stabilization training on balance and motor patterns in a patient with Charcot- Marie-Tooth disease. Neuroendocrinol. Lett. 33, 101e108.
53. Kolar, P., Sulc, J., Kyncl, M., Sanda, J., Cakrt, O., Andel, R., Kumagai, K., Kobesova, A., 2011. Postural function of the diaphragm in persons with and without chronic low back pain. J. Orthop. Sports Phys. Ther. 42, 352e362.
54. Koĺar, P., Kobesova ́, A., 2010. Postural e locomotion function in the diagnosis treatment of movement disorders. Clin. Chiropractic 13, 58e68.
56. Clare Frank, Alena Kobesova, Pavel Kolar Dynamic Neuromuscular Stabilization, and Sports Rehabilitation. The International Journal of Sports Physical Therapy Volume 8, Number 1 February 2013 Page 62
57. Tsao H, Hodges PW. Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. J Electromyogr Kinesiol 2007, in press.
58. Tsao H, Hodges PW. Immediate changes in feedforward postural adjustments following voluntary motor training. Exp Brain Res 2007;181(4):537–46.
59. Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine 1996;21(23):2763–9.
60. Danneels LA, Vanderstraeten GG, Cambier DC, et al. Effects of three different training modalities on the cross-sectional area of the lumbar multifidus muscle in patients with chronic low back pain. Br J Sports Med 2001;35(3):186–91.
61. Rissanen A, Kalimo H, Alaranta H. Effect of intensive training on the isokinetic strength and structure of lumbar muscles in patients with chronic low back pain. Spine 1995;20(3): 333–40.