Dysbiosis and Leaky Gut

In the last article, we explored metabolic syndrome and its relationship to musculoskeletal inflammation and pain. This month, we are looking at another hidden source of inflammation: the gastrointestinal system. “Dysbiosis” and “leaky gut” are the source of many long-standing and elusive syndromes in patients such as chronic fatigue, fibromyalgia, and irritable bowel syndrome; as well as, familiar autoimmune disorders like rheumatoid and psoriatic arthritis, multiple sclerosis, and ankylosing spondylitis.
First, let’s define leaky gut and dysbiosis, and look at the ways this will impact the patients’ immune system and ultimately inflammation and pain. Then we will explore the primary laboratory study used for assessment. Finally, a short review of some treatment options, including a personal protocol I have found very successful for some patients.
Before plunging headlong into definitions, please understand your patient may not have any intestinal symptoms. However, with a couple probing questions I am usually able to elicit the truth. Even though patients don’t like to talk about their bowel habits, ask the patient three things: Do you have gas, bloating or abdominal pain? Do you feel overly full for an extended time after a meal? Do you have a bowel movement every day? More than likely you will find something of significance. By the way, people should have bowel movements daily, and typically more than once a day. You wouldn’t let your trash pile up for a few days before removal, would you?
Healthy arrays of bacteria populate all of our gastrointestinal systems. A similar assortment is also taking up residence in our orodental, respiratory, genitourinary, and integumentary systems, and although not the purpose of this article, these other loci of bacterial colonization must not be ignored as a source of potential disruption for the patient. Regarding the GI, when this collection gets out of balance or a foreign invader occupies the territory problems will persist. Most of the time, this is not an acute issue for the patient such as gastritis or colitis.
Dysbiosis occurs when the friendly lineup of bacteria becomes offensive in nature. Much like a team, the flora of the gut is the defensive team for your GI system which faces an offense that can obliterate it. As far back as 1939, “auto-intoxication” was described in the medical literature as intestinal in origin, and treatments ranged from dietary changes and supplements to colonic irrigation. What we know now is that endotoxin from imbalanced bacteria, particularly gram-negative, causes an increase in the nuclear factor kappa B (NFkB), which launches immune dysfunction and inflammation throughout the system, eventually leading to pain.
Vasquez further subdivides dysbiosis into insufficiency, overgrowth, immunosuppressive, hypersensitivity/allergic, inflammatory and reactive arthritis, and parasites:
- Insufficiency – this lack of “good bacteria” interferes with digestion, absorption, and elimination;
- Bacterial overgrowth – too many of the “bad guys,” yeast and bacteria. This is the cause of most irritable bowel and fibromyalgia. Increased permeability or “leaky gut” leads to immune complex formation and inflammation begins. Please remember the mucosa (gut) associated lymphoid tissue (MALT/GALT) that surrounds the intestines comprises 60% or more of the immune system. 40% of rheumatoid patients have bacterial overgrowth in the small intestine;
- Immunosuppressive – Candida albicans can release toxins that are immunosuppressive in nature;
- Hypersensitivity/Allergic – Candida and certain bacteria can cause an immune reaction in some patients that resembles allergy. These bacteria have to be eradicated and replaced in these patients;
- Reactive arthritis – people with certain genetic tendencies will react to bacteria causing reactive arthritis. The most common being Reiter’s HLA-B27 after exposure to Chlamydia trachomatis. Proteus mirabilis is associated with rheumatoid arthritis, Streptococcus sp. and Staphylococcus sp. are associated with psoriasis and psoriatic arthritis; and
- Parasites – these are not necessarily helminthes, but may be bacteria which do not belong in the gastrointestinal tract.
How does imbalance occur? It can start as early as childhood. Breastfeeding encourages good bacterial growth from the beginning. However, vaccinations, antibiotics, prednisone, and other medications, as well as, poor lifestyle choices such as processed foods and refined carbohydrates contribute to unhealthy inhabitants. Add other complicating factors such as travel to foreign countries, food poisoning and other potential infections and these unwelcome intestinal guests can cause gas, bloating, pain, constipation, and diarrhea at the local level, and globally, fibromyalgia, autoimmune disorders, arthritis, and chronic fatigue.
As far as the assessment is concerned, the comprehensive stool analysis is the most reliable choice for really understanding any imbalances. One caution: stool analysis is not always a perfect science. If patients present with obvious gut issues, start them on an anti-inflammatory treatment plan before testing. Sometimes, just taking the most likely offending substances (i.e. gluten, sugar, and dairy) out of the diet will alleviate most of the patients’ issues. However, stool analysis can yield other important information:
- Beneficial and harmful bacteria/yeast count – A stool analysis will give you an idea of what is growing in the patients’ intestines. You will have a clear understanding of whether there is an imbalance or not and whether it is overgrowth, insufficient growth or both.
- Sensitivity Testing – This will give you a list of effective natural and prescription anti- microbial agents for particular yeast or bacteria.
- Beta-glucuronidase – High levels indicate the need to restore the “good guys.” The B-glucuronidase breaks down toxins that the liver has already conjugated and returns them to the system via enterohepatic circulation.
- Short Chain Fatty Acids (SCFA) – Produced by bacteria in the intestines, and aids in the differentiation of overgrowth (too many SCFA) versus insufficiency (too few SCFA)
- Secretory IgA – Immune responses to flora or food elevate these levels, while low levels indicate a stunted immune response may be secondary to medications (prednisone), malnutrition, bacterial immunosuppression, and stress.
- Lactoferrin – A direct inflammatory marker used to distinguish between inflammatory bowel disease and irritable bowel syndrome.
These are the most common markers. The stool test will give you valuable information before starting treatment or when treatments are ineffective.
Treating the patient with dysbiosis and leaky gut is very rewarding when they are motivated to change their food and lifestyle. My experience is that long term IBS can virtually disappear in a week when patients are compliant. Of course, an anti-inflammatory modified Mediterranean diet is optimal for most patients. Patients with gluten free, dairy free diets for at least 90 days will help starve the microbes. Diets without refined carbohydrates, sugar, and dairy will reduce the antigenic load and provide less “food” for the bad bugs. Patients are more compliant when we remind them that the modified diet is not forever. Reminding them WHY they are following the plan is also helpful.
The most efficient plan for these patients involves a 28-day anti-inflammatory program to kick-start their healing. Several different companies offer this type of plan. Personally, I like to combine InflammaCore (OrthoMolecular) or UltraInflamX (Metagenics), 2 scoops BID, titrated to patient tolerance over the first week, and Pro-225 (for 15 days – OrthoMolecular) with the 28-day elimination diet from Metagenics. These patients are seen weekly to insure compliance, and we can adjust the dose of the InflammaCore if necessary. Some patients can only tolerate 1-1.5 scoops BID.
For overgrowth, natural antimicrobial can be quite effective and easily chosen based on the results of the stool analysis. CandiBactin AR and/or BR (Metagenics) or Intestinol and/or Candicin Forte (OrthoMolecular) are great choices. Experience has taught me that most people don’t take enough of these natural anti-microbial agents to be effective. Instead, you may recommend dosing BID or TID up to twice the recommended amount for 3-6 months, as treating with less for shorter amounts of time will not be as effective in the long run. If you are using a combination of two supplements, lower the doses of both.
The most common substances include:
- Oregano Oil – 600+mg per day for at least 6 weeks
- Berberine – 400+mg per day. Berberine also has glucose and blood pressure lowering effects, and it is anti-inflammatory as well. I recommend about twice this amount for the first two weeks.
- Artimisia annua – 100 mg BID in conjunction with another herbal like Berberine.
- UvaUrsi – particularly good for UTI, but depending on the sensitivity, may also be highly effective for GI issues.
- Thyme
- Clove – as an anti-fungal
- Caprylic Acid and undecyclenic acid – for yeast
Cleaning up the gastrointestinal system may seem complicated, but do not be overwhelmed. Reducing chronic pain and inflammation originating in the gastrointestinal system will make your chiropractic care much more effective. Patients will suffer less, and this may be the first time in their life that their GI system is functioning the way it was designed. The body has incredible recuperative potential, our job is to lead the patients to the right switches and turn on the power. It’s a win for everyone. As always I am available to field any questions about this or any of my other articles.
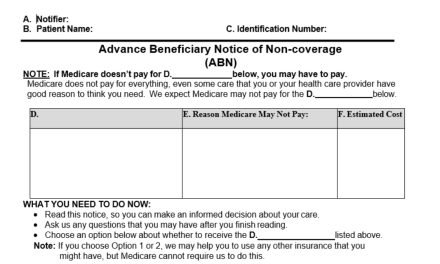
Editor’s Note: As always, please read the medical policies of the insurers with whom you are contracted to determine insurance coverages and requirements. Additionally, review these insurance coverages with your patients.