Conservatively Managing Meniscus Lesions

Introduction
The knee menisci are shock-absorbent, fibrocartilage discs which conform to the femoral and tibial intraarticular contours. The medial and lateral menisci are both affixed to the superior articular surface of the tibia through anterior and posterior bony attachments. (1) The peripheral one-third of a meniscus (near its capsular attachment) is vascularized and innervated for pain and proprioception. The remainder of the meniscus is avascular and lacks nerve supply. (2,3) Not surprisingly, healing potential diminishes in the less vascular inner region. (28)
The menisci play an important role in knee biomechanics. The menisci transmit 50-70% of compressive loads in full knee extension and up to 85 percent at 90 degrees of flexion. (4) The lateral meniscus is thought to play a greater role in load transmission, while the medial meniscus provides greater stability, particularly as a secondary restraint to anterior tibial translation. (5,6) The menisci move posteriorly during knee flexion from 0-120 degrees, with the medial meniscus translating 5.1 mm and the lateral meniscus retreating up to 11 mm. (7) Other mechanical duties include shock absorption, prevention of synovial impingement, synovial fluid distribution and lubrication. (1)
Meniscal injuries are common, affecting 60-70 per 100,000 persons annually. Males are affected more frequently at a rate of 3 or 4:1.(3) Meniscal tears may be classified as “traumatic” or “degenerative.” Meniscal injuries may occur at any age. In children and adolescents, the menisci are durable and rubbery, so most injuries are “traumatic” as a result of a forceful rotational injury. As we age, the meniscus grows weaker and “degenerative” tears become more likely, often resulting from simple or unrecognized insults. (1,3,9) “Degenerative” tears are more common. (1,3) The medial meniscus is damaged more commonly than the lateral meniscus, with acute tears often involving the middle and posterior regions. (1)
In addition to classifying meniscal injuries as traumatic or degenerative, they may be further classified according to the pattern of tear. Eighty percent of tears are classified as either “vertical” (flap, parrot beak, bucket handle) or “oblique.” (3) “Radial” (transverse) tears disrupt the circumferential fibers of the meniscus and occur more frequently in the lateral meniscus. (9) “Longitudinal” tears are common in the medial meniscus. Additional tear patterns include “horizontal” and “complex.” Acute meniscal injury may accompany fracture or ligamentous injury. Approximately one-third of meniscal tears are associated with ACL injuries. (9,10)
Clinical Presentation
The typical presentation for meniscus injury is somewhat dependent upon the age of the patient. Young patients often present following a traumatic insult, particularly a sudden twist on a loaded knee. Following acute injury, the patient may have difficulty with full weight-bearing and may demonstrate an altered gait. Older patients with degenerative injuries may not be able to report an inciting event. Patients of any age usually complain of intermittent, movement-related pain, chiefly upon deep knee bends. Clicking, catching or locking, particularly between 20-45 degrees of extension, is common. The patient may report a sensation of giving-way or buckling.
The presence of joint line tenderness, corresponding to the site of injury, may be one of the most reliable indicators of a tear. (74% sensitivity, 50% specificity). (3) Palpation may demonstrate signs of increased synovial fluid production, including cysts at or below the joint line, and swelling of the popliteal bursa (i.e., Baker’s cyst). Palpation of the medial meniscus is enhanced by knee flexion and internal tibial rotation, and for the lateral meniscus with flexion and external rotation. (27) Range of motion may be limited in flexion or extension. Displaced (vertical or bucket handle) tears may present as a rubbery movement block. Terminal knee flexion or deep squatting is frequently uncomfortable. Circumduction testing of the knee commonly elicits pain. (11)
The most sensitive orthopedic test for the detection of meniscal injury is the Thessaly test at 20 degrees of knee flexion with a diagnostic accuracy of 94-96%. (12) The Thessaly test is performed with the patient standing flat-footed on the affected leg, in front of the clinician, arms outstretched and supported by the clinician. The patient squats to flex their knee to 20 degrees and then rotates their trunk internally and externally. Reproduction of discomfort or catching constitutes a positive test. Another weight-bearing test for meniscus damage is Ege’s test, performed as follows: the patient stands shoulder-width apart and slowly squats, first with legs in maximal external rotation (to test the medial meniscus), and then with legs in maximal internal rotation (to test the lateral meniscus). Pain, clicking, or locking suggests meniscus tear. The test shows good sensitivity (64-67%) and specificity (81-90%) and is more accurate for detecting non-degenerative tears. (26)
McMurray’s sign is performed on a supine patient with the hip and knee flexed to 90 degrees. The examiner passively extends the patient’s knee with the foot internally and externally rotated while palpating the joint lines for a “clunk.” Discomfort with this maneuver is common, but a true positive test requires a clunk and is rare, but extremely specific, when present. (3)
Imaging
Plain film weight-bearing radiography may be needed to rule out fracture, osteochondral lesions, loose bodies, and degenerative changes. (1) The Pittsburg Knee Rules are 99% sensitive for detecting fracture and state that radiographs are warranted with a mechanism of injury, including blunt trauma or a fall, AND any of the following: age < 12, age >50, or inability to walk four weight-bearing steps. (30) Alternately, the Ottawa Knee Rules state that an X-ray is required to rule out fracture only in patients who have an acute knee injury with one or more of the following: age 55 years or older, tenderness at head of fibula, isolated tenderness of patella, inability to flex the knee greater than 90 degrees, or inability to bear weight both immediately and in the emergency department for 4 steps. (31)
MRI is the most sensitive imaging modality for evaluation of menisci, but interpretation of MRI findings with regard to meniscal injuries may be confusing, and false positives are common. MRI exams reveal clinically irrelevant signal alterations or tears in 30-36% of asymptomatic patients. (13,29) Routine MRI imaging should be reserved for patients in whom arthroscopic surgery is anticipated. (14)
Management
Chiropractors can play an important role in the rehabilitation of most degenerative and some traumatic meniscal injuries. Although the majority of acute tears in a young population will require surgical intervention, one-third of these injuries may be treated conservatively with full resolution. (16) Acute tears most amenable to conservative care include peripheral radial tears less than 5 mm and longitudinal tears along the posterior horn of the lateral meniscus. (17) Acute tears associated with joint locking warrant surgical referral.
For older patients with degenerative tears, a trial of conservative therapy is generally appropriate. The patient’s age roughly correlates with the need for surgical intervention. Only about 6% of patients over the age of 40 require operative management. (18) Patients with manageable pain and swelling, without loss of joint function, have shown functional improvement through conservative care equal to those who have undergone arthroscopic surgery. (19,32)
Initial conservative management should include rest, ice, compression and elevation (RICE). Activity modification is essential to prevent further damage. Patients should avoid twisting on a weight-bearing, flexed knee and may need to temporarily or permanently discontinue high-energy sports activity, like soccer or tennis. In some instances, a brace may be necessary to limit motion. Ice and anti-inflammatory modalities may help limit inflammation. NSAID’s may be appropriate in the initial stages. (20)
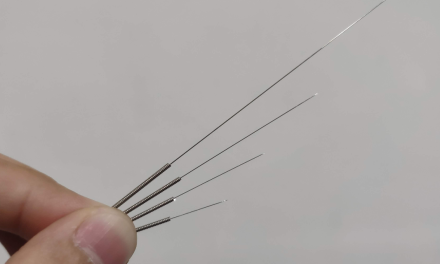
Stretching and myofascial release techniques may be necessary for the hamstring, adductor, quadriceps, gastroc, soleus and popliteus muscles. IASTM of the knee capsule may provide benefit, as the meniscus has a shared attachment with this structure. Manipulation may be necessary for restrictions in the ankle mortise joint, fibular head, hip, sacroiliac joints, and spine.
Stationary bicycling, water walking and isometric strength training may be incorporated as swelling decreases. Later, dynamic exercises should include single-leg calf raises, knee flexion, knee extension and lunges above 80 degrees of knee flexion. (21) Biomechanical deficits in hip or knee stability should be addressed, particularly gluteal weakness and patellofemoral tracking disorders. Arch supports or orthotics may be necessary for patients who overpronate.
Patients who require surgical repair may also benefit from a well-planned home exercise program. Rehab goals following partial meniscectomy include reduction of pain and inflammation with restoration of range of motion, strength, and function. Restoration of pre-operative quadriceps and hamstring strength is essential. (22) Post-arthroscopic rehabilitation should progress through the aforementioned exercises as tolerated, avoiding torsion to a flexed and loaded knee.
Surgical removal of meniscal tissue results in increased bony contact between the tibia and femur. (7) Degenerative changes develop in nearly all post-meniscectomy patients. (24) Degeneration seems to more common in those who have undergone lateral meniscectomy. (25)
About ChiroUp
ChiroUp provides up-to-date and easy-to-access resources to help evidence-based chiropractic physicians deliver effective and patient-centric care. Their mission is to enable doctors of chiropractic to achieve exceptional clinical outcomes and promote their brand of excellence to patients, physicians, and healthcare decision-makers.
References
- Goldblatt JP, Managing meniscal injuries: The diagnosis. J Musculoskel Med. 2009;26:343-351
- Arnoczky SP, McDevitt CA. The meniscus: structure, function, repair, and replacement. In: Buckwalter JA, Einhorn TA, Simon SR, eds. Orthopaedic Basic Science: Biology and Biomechanics of the Musculoskeletal System. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2000:531-545.
- Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury, I: basic science and evaluation. J Am Acad Orthop Surg. 2002;10:168-176
- Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34:252-257.
- Packer JD, Rodeo SA. Meniscal allograft transplantation. Clin Sports Med. 2009:28:259-283, viii.
- Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg. 1982;64A:883-888.
- Simon SR, Alaranta H, An KN, et al. Kinesiology. In: Buckwalter JA, Einhorn TA, Simon SR, eds. Orthopaedic Basic Science: Biology and Biomechanics of the Musculoskeletal System. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2000:730-827.
- Klimkiewicz JJ, Shaffer B. Meniscal surgery 2002 update: indications and techniques for resection, repair, regeneration, and replacement. Arthroscopy. 2002;18:14-25.
- Kilcoyne KG et al Epidemiology of meniscal injury associated with ACL tears in young athletes”; The Cutting Edge, OrthoSuperSite; March 2012
- Levy IM, Torzilli PA, Gould JD, Warren RF. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg. 1989;71A:401-406.
- Karachalios T, Hantes M, Zibis AH, et al. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Joint Surg. 2005;87A:955-962.
- Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34:252-257.
- Miller GK. A prospective study comparing the accuracy of the clinical diagnosis of meniscus tear with magnetic resonance imaging and its effect on clinical outcome. Arthroscopy. 1996;12:406-413.
- Ciliz D, Ciliz A, Elverici E, et al. Evaluation of post-operative menisci with MR arthrography and routine conventional MRI. Clin Imaging. 2008;32:212-219
- Goodwin Peter C, Effectiveness of supervised PTin the early period after arthroscopic partial menisectomy. Physical Therapy, 2003;83(6): 520-535.
- Saidoff David, McDonough Andrew. Critical Pathways in therapeutic intervention. Extremities and Spine; Philadelphia, PA: Mosby Inc., 2002: 611-639.
- Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy 1998;14:824–9.
- Rimington T, Mallik K, Evans D, Mroczek K, Reider B. A prospective study of the nonoperative treatment of degenerative meniscus tears. Orthopedics 2009;32:8.
- Lim HC, Bae JH, Wang JH, Seok CW, Kim MK. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 2010;18:535–9.
- Havard Osteras, Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 24 August 2006
- Matthews P, St-Pierre DM. Recovery of muscle strength following arthroscopic meniscectomy. J Orthop Sports Phys Ther. 1996;23:18–26
- Andersson-Molina H, Karlsson H, Rockborn P. Arthroscopic partial and total meniscectomy: a long-term follow-up study with matched controls. Arthroscopy. 2002;18:183-189.
- Salata MJ. A Systematic Review of Clinical Outcomes in Patients Undergoing Meniscectomy. American Journal of Sports Medicine. 2010 vol. 38 no. 9 1907-1916
- Akseki D, Ozcan O, Boya H, Pinar H. A new weight-bearing meniscal test and a comparison with McMurray’s test and joint line tenderness. Arthroscopy, 2004;20(9):951-958.
- Chivers M, Howitt S. Anatomy and physical examination of the knee menisci: a narrative review of the orthopedic literature. J Can Chiropr Assoc, 2009;53(4):319-333.
- Jeong H, Lee S, Ko C. Meniscectomy. Knee Surg Related Res, 2012;24(3):129-136.
- Ryzewicz M, Peterson B, Siparsky P, Bartz R. The diagnosis of meniscus tears. Clin Orthop Related Res, 2007;455:123-133.
- Seaberg, David C. et al. Clinical decision rule for knee radiographs. The American Journal of Emergency Medicine, Volume 12, Issue 5, 541 – 543
- Stiell IG et al. Implementation of the Ottawa Knee Rule for the use of radiography in acute knee injuries. JAMA 1997 Dec 17;278(23):2075-9.
- van de Graaf VA, Noorduyn JCA, Willigenburg NW, et al. Effect of Early Surgery vs Physical Therapy on Knee Function Among Patients With Nonobstructive Meniscal TearsThe ESCAPE Randomized Clinical Trial. JAMA.2018;320(13):1328–1337. doi:10.1001/jama.2018.13308