Medicare Billing Explained for Participating, Non-Participating, Assigned, and Non-Assigned Claims
The Medicare Fee Schedule revolves around three key amounts: fees allowed for participating providers, fees allowed for non-participating providers, and the limiting charge. Discover more by watching the video!
Transcript:
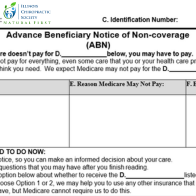
Over the years, we’ve received a number of questions and calls regarding the Medicare fee schedule, and trying to understand the differences and all the different numbers. And really, it boils down to three sets of numbers. It’s the allowable charge for participating providers, it’s the allowable charge for non-participating providers, and the limiting charge. Everything is really based on those three figures.
So the way the fee schedule works is it utilizes the allowable charge for a participating provider as the baseline. So if that charge were to say, would it be $100, then of course, you would charge either $100 or your standard office fee, whichever is a lesser amount. And so if you’re a participating provider, that really is easy. For participating providers, you can charge your normal office fee, and Medicare will adjust that down to that to that allowable amount through the remittance advice process or through the EOB process. But then, where things get confusing a bit is when we move into that non-participating realm. And so the way that nonparticipating allowable charge works is it is 95% of the allowable charge for the participating providers. So in our example of $100, then for a non-participating provider, the allowable charge would be $95.
Now, the limiting charge is different. The limiting charge is what a doctor who is not accepting assignment from Medicare can charge the patient, they will cap that amount, so you can’t charge $200 In our example, that doesn’t work. The way it works is they they establish a maximum charge that a non-participating provider who does not accept assignment can charge the patient and it is 15% higher than the non-participating allowable amount. So in our case, at $95 15%, higher is $109.25. So it is a higher amount than what an allowable charge is for a participating provider with Medicare. But the patient’s responsibility is then going to be greater. And that can come into into affected when you’re when you’re convincing a patient of your services, or it may not make a difference because the patient very well may have secondary insurance, or they may have supplemental Medicare insurance that covers that difference anyway. So that is the biggest difference. So the baseline is your Medicare participating provider allowable charge, and then 95% of that is the allowable charge for a non-participating provider and the limiting charge is the maximum that they can pay or then the maximum that a non-par doctor can charge the patient, and that is 15% higher than that non participating allowable charge.
Now Medicare will only pay 80% of the allowable charges for the higher amount for a participating provider or the lower amount for a non-par provider. Now this is a really important nuance that I think sometimes gets lost. That limiting charge is only applicable when you are not accepting assignment. So if you’re a non-par doctor that is accepting assignment, that limiting charge no longer matters, you can only charge the patient for the difference between the allowable charge for the participating provider and the amount that Medicare is going to cover that 20%. And so that is a very important thing you cannot charge up to that limiting charge if you are choosing to accept assignment.
So if you’re a non-par doctor and you’re accepting assignment, checking the assignment box, then you cannot charge up to the limiting charge, you can only charge the patient for that 20% difference for that Medicare nonparticipating allowable charge. So in our example of $95 per se, then the maximum amount that you would be able to charge that patient is $19. And then Medicare will reimburse you the difference between 95 and $19 or $76, as the case might be, and so that is how that plays out. Hopefully, that explains the fee schedule and the difference in par and non-par providers. Remember we cannot as chiropractic physicians, we can not opt out of Medicare. You have to be either participating or non-participating or not see a Medicare patient at all. Hopefully, this information helps you out and we’ll catch you next week.