Radiology of Osteonecrosis
Osteonecrosis, or the death of bone tissue, can be a source of pain and eventual possible long-term disability. There may be an underlying condition that may predispose to altered vascular supply to the bone, or, in many cases, the cause is undetermined and is termed idiopathic. The severity of any long-term sequela is largely determined by the location of the focus of osteonecrosis. The epiphysis, metaphysis or diaphysis may be involved. Because of the importance of the epiphysis in joint integrity, a focus of involvement in this area can have devastating functional consequences.
As mentioned above, there are a variety of predisposing conditions that can have osteonecrosis as a result. I will present a short list of conditions that should be screened for if this diagnosis is suspected (1):
Trauma
A fracture or dislocation that impairs the vascular supply to a part of a bone. Common areas of involvement include the epiphyses of the femoral and humeral heads, talus and scaphoid.
Corticosteroids
An endogenous or exogenous increase in corticosteroid levels in the blood stream have a known correlation with the development of osteonecrosis. This may be due to the development of fat emboli in the blood stream with vessel occlusion.
Hemoglobinopathies
Sickle cell anemia is probably the most common of this group. The formation of abnormally shaped red blood cells may affect the flow through vessels and lead to occlusion. This is most commonly noted in the hands and feet.
Collagen Diseases
Rheumatoid arthritis and systemic lupus erythematosus (SLE) are common examples. A vasculitis is associated with these conditions that can lead to the formation of thrombi and subsequent infarction.
Spontaneous
This is the most common cause of osteonecrosis. The precise mechanism in this case is not identified. As opposed to the previous etiologies, this type of involvement is usually solitary and does not involve more than one bone. The bones most commonly affected in this category are the femurs, metatarsals and lunate.
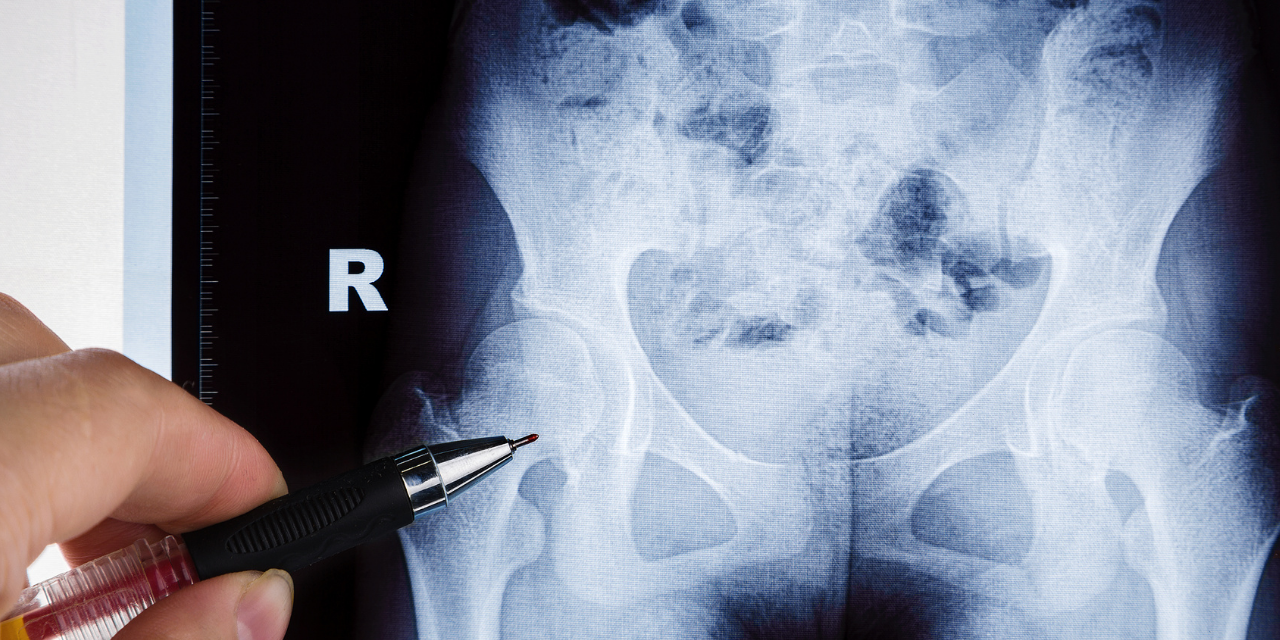
Depending on the site of involvement, the radiographic appearance of osteonecrosis can vary. When involving the femoral epiphysis, for example, there may be femoral head collapse, a fragmented appearance to the head, disruption of the trabecular pattern, increased density of the head, the formation of subchondral cysts and eventual subchondral fracture.
With involvement of the metaphyseal or diaphyseal aspects of the bone, the early radiographic appearance is one of focal bone density loss. This area later develops a calcified rim and a mottled or septated appearance within the lesion. The border often has an undulating contour that is termed serpiginous and is pathognomonic of the lesion.
Plain film radiography is often unrewarding in the early stage of the lesion. MRI examination will show findings much earlier than plain film x-ray and will demonstrate high signal within the lesion on the T-2 or fat suppressed images (2). This high signal area may be surrounded by a thin rim of low signal. Radionuclide bone scans will show increased uptake in the region of the lesion, although this modality has been largely supplanted by MRI.
Images 1, 2 and 3 demonstrate various appearances in the hip. Figure 1 features a degree of articular collapse of the right femoral head. In figure 2 there is a mottled appearance of the left femoral head without obvious articular collapse. Figure 3 combines a dense mottled appearance of the head with obvious articular collapse. A similar appearance is noted in the right shoulder (Figure 4).




An MRI image of the right knee is seen in Figure 5 (fat suppressed sequence). The medial femoral condyle displays diffuse high signal intensity. The articular cortex has not been affected at this point and remains intact.

Figures 6 and 7 represent MRI images of the shoulder. In figure 6, a well-defined lesion with a low signal intensity border is seen subcortically in the superior aspect of the humeral epiphysis. Figure 7 demonstrates a high signal intensity lesion in the humeral dia-metaphysis with a low signal intensity serpiginous border.


Figure 8 is indicative of a more mature infarct in the proximal humerus, featuring a predominantly mottled sclerotic appearance.

In conclusion, osteonecrosis of bone is a lesion that in certain instances may be amenable to diagnosis with plain film x-ray. MRI will exhibit findings much earlier than x-ray in general. Patients exhibiting a pain pattern that is rather nondescript, particularly if underlying predisposing conditions are identified, should be imaged in a timely manner. Diagnosis of this condition as early as possible is essential in avoiding long-term complications.
References
- Yochum T.R., Rowe L.J.: Essentials of Skeletal Radiology, ed 3. Philadelphia, Lippincott Williams & Wilkins, 2005
Stoller D.W.: Magnetic Resonance in Orthopaedics and Sports Medicine, Philadelphia, Lippincott Com