Omohyoid Syndrome

A 59-year-old female presented on referral from her family physician for complaints of left anterior neck pain. Duration of symptoms was three weeks and began suddenly. Onset was directly caused by a soft tissue strain resulting from a mechanical fault in the vehicle she was driving. While driving on a curvy road, the accelerator stuck and the vehicle continued to increase speed. The vehicle speed reached 80 mph before she thought to turn off the ignition and engage the emergency brake. As a result of the increased speed, the curvy nature of the road and the stress of the situation, she was left with a strain to the left anterior aspect of the neck. Ibuprofen and muscle relaxants failed to adequately relieve her pain and she was referred for chiropractic evaluation and treatment. On examination, palpation revealed pain and a positive jump sign at the left sternocleidomastoid muscle near its attachment (but slightly lateral and superior) to the clavicle. The omohyoid muscle was exquisitely tender with a trigger point and a boggy, swollen feeling. With the exception of limited cervical extension, ROM was actively and passively normal but accompanied by mid-range and end-range pain. Subjective pain level was 7. Mobility of the sternoclavicular joint was normal. Deep tendon reflexes, upper extremity motor testing and dermatomal examination were all normal. No constitutional symptoms reported.
Diagnosis
Cervical Strain – Specifically Omohyoid Syndrome. Treatment was initiated with: myofascial release; post-isometric contraction-relaxation stretching technique; pre-modulated electrical stimulation technique; and cold packs. As pain levels dropped, cervical spine strengthening was performed on a cervical 4-way apparatus against weighted resistance. The patient was discharged after 9 treatment sessions with no further reports of pain.
Follow-Up
In his book, Atlas of Uncommon Pain Syndromes 2nd Ed, Waldman discusses a pain management approach to treating omohyoid syndrome. This approach brings with it a host of potential complications including brachial plexus and phrenic nerve injury secondary to misplacement of the needle. He warns clinicians to be thorough in considering the diagnosis as missed diagnoses can include hyoid bone fracture, occult cervical fracture, tumors, and pharyngeal disease can all give rise to similar symptoms.
Clinical Pearl
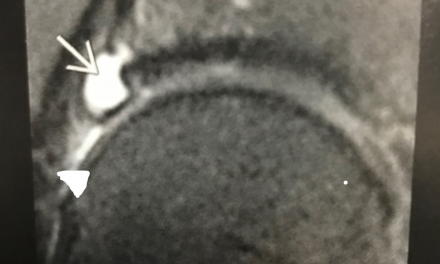
Swelling and tenderness in the left supraclavicular area should raise clinical suspicion. A large swollen lymph node in this region is referred to as a Virchow’s node. Malignancies of the internal organs can reach an advanced stage before giving symptoms. Stomach cancer is often without symptoms while it metastasizes. One of the first visible spots where these tumors metastasize is the left supraclavicular lymph node. Many clinicians feel that Virchow’s node is pathognomonic for abdominal (typically stomach) malignancy and this notion warrants thorough examination to rule out. Submitted by David W. Flatt, DC, DABCO. Dr. Flatt is a board certified chiropractic orthopedist and a Partner at Greater Valley Medicine in St. Charles, Illinois.