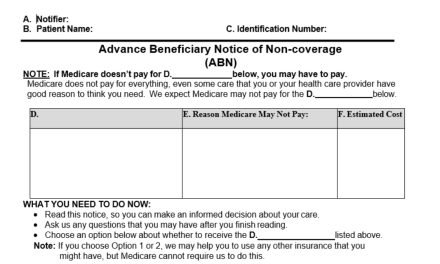
Hydroxyapatite Deposition in the Spine

Plain film radiographs often reveal calcifications in or near the spine. These calcifications, while generally relatively common and innocuous, may at times be symptomatic. One type that occurs fairly frequently is the result of degenerative changes. A second variety, while painful, should not be a major cause for concern. We will explore that symptomatic variety first.
Although the etiology is not well understood, at times there may be deposition of hydroxyapatite crystals within the longus colli musculature adjacent to the anterior surface of the cervical spine vertebral bodies. This is most commonly seen inferior to the anterior tubercle of the atlas, although less frequently it may be seen at other cervical levels (1). The calcification itself is sometimes not well defined; however, generally, it measures less than 2 cm. in diameter and is best seen on the lateral projection. Frequently there is an increase in the retropharyngeal space locally. Muscle spasm may result in a reduction of the lordosis. Figure 1 demonstrates the calcification anterior to the base of the dens on the lateral projection. The arrow points to the calcification, while the arrowheads delineate the anteriorly displaced margin of the retropharyngeal space.

On MRI examination, the water-sensitive sequences will demonstrate high signal intensity at the superior aspect of the longus colli muscle, representing edema. The calcification itself will display decreased signal intensity on all sequences.
Symptoms are self-limiting and include muscle spasm, pain, and stiffness in the neck, difficulty swallowing and a sense of globus hystericus. The symptoms usually resolve within 1-2 weeks. With resolution of the symptoms, there is also resorption of the calcification and eventual disappearance radiographically.
Other causes of spinal calcification include the relatively common degenerative types and much less frequently are the result of rare conditions such as ochranosis, hemochromatosis, hyperparathyroidism, hypervitaminosis D and gout. There some cases of idiopathic discal calcification.
Calcification of the intervertebral disc may involve either the nucleus pulposis or the anulus fibrosis. When due to degeneration, the calcifications will accompany other more traditional degenerative changes: decreased disc height, osteophyte formation, and endplate sclerosis. Calcifications within the nucleus are generally round or flattened in shape. These calcifications may be subtle and not obvious on plain film.
Calcification of the outer anular fibers may occur. These generally occur at the periphery of the disc and are vertically oriented and curvilinear in shape. Usually these are noted anteriorly in the disc space; however, they may sometimes be seen laterally. They usually are not continuous with the vertebral body. Figure 2 demonstrates an anterior anular calcification in the cervical spine with adjacent osteophyte formation. These are sometimes referred to as “intercalary ossifications.” Symptoms in the spine are not directly referable to these calcifications but rather to the underlying degenerative changes.

Idiopathic disc calcification may be found in childhood and adulthood. They involve only the nucleus pulposis and not the anulus fibrosis.
The childhood idiopathic variety is most commonly seen in the cervical spine and manifests between the ages of 6 and 12 years. Involvement of a single disc is most common. The calcification is usually a flattened oval shape with a mildly widened intervertebral disc space. Figure 3 displays an interdiscal calcification at the C3-C4 level The majority of these patients will have associated pain. The symptoms gradually resolve over a period of weeks, as does the disc calcification.

Adult idiopathic disc calcification is sometimes observed; however, the patients are asymptomatic. In reality, these calcifications may be a manifestation of degenerative disc disease, but there is a lack of concurrent spinal degenerative findings.
In addition, there may be calcification within a sequestered disc fragment. If this herniation occurs posteriorly at the disc, the fragment may be extruded into the spinal canal. Calcification of this extruded fragment may be visible on x-ray and be symptomatic.
Disc calcifications are a relatively common phenomenon, and some care needs to be exercised in deciding whether symptomatology may be attributable to them.
References
- Yochum T.R., Rowe L.J.: Essentials of Skeletal Radiology, ed 3. Philadelphia, Lippincott Williams & Wilkins, 2005.
The attached images in this article were graciously provided by Dr. Terry Yochum DC, DACBR and are found in the above referenced “Essentials of Skeletal Radiology.”
Douglas Gregerson DC, DACBR is the chief radiologist for Gregerson Radiology Consultants, website www.mychiropracticradiologist.com.