Spontaneous Osteonecrosis as An Etiology for Knee Pain

An infrequent source of knee pain is spontaneous osteonecrosis of the knee (SONK). Osteonecrosis is often the result of pre-existing factor; however, when there is no underlying cause, it is presumed to be spontaneous. Pathologically, a focus of infarction occurs subchondrally in the weight-bearing portion of the bone. The medial condyle of the femur is the most frequent site of involvement in the knee, although the lateral femoral condyle or medial tibial plateau may infrequently be involved. SONK is a separate entity from osteochondritis dissecans, which is a disorder of adolescents and has a different set of clinical and radiologic findings, as well as a different pathology.
SONK most frequently occurs over the age of 60 and is slightly more common in females (1). Symptomatically, there is a sudden onset of knee pain, with increasing severity. On clinical examination, tenderness of the medial femoral condyle may be present, sometimes with knee joint effusion.
Radiographically, there will likely be no findings initially on plain film. It may take 5-6 weeks for the initial radiographic findings to appear. These findings may manifest as a focal area of subchondral sclerosis, and, if not diagnosed and treated early on, articular surface collapse may occur later. Figure 1 demonstrates late-stage involvement with articular collapse.

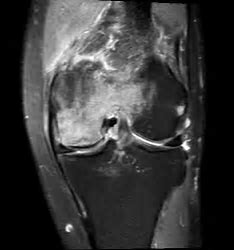
MRI is a vastly more sensitive imaging tool for the early visualization of this condition and has a sensitivity rate of 98% for early detection. Fat suppressed images are particularly useful, with increased intraosseous signal intensity surrounding a focus of crescentic low signal intensity. The low signal intensity represents the area of the trabecular fracture, with high signal intensity edema surrounding it. Identification of the low signal subchondral fracture line is the key to this diagnosis, as other conditions may also manifest intraosseous edema. T-1 weighted images will show rather more uniform low signal intensity, and the sharp fracture line may not be as easily discernable.
Figure 2 is a fat-suppressed coronal image, with typical high signal intensity representing surrounding intraosseous edema in the epiphysis of the medial femoral condyle. Adjacent to the articular surface is a low signal intensity serpiginous/crescentic line that represents the collapsed trabeculi.
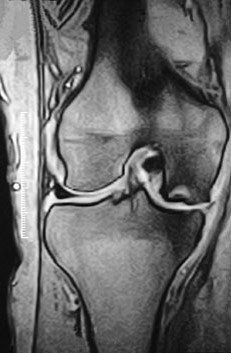
A T-1 weighted sagittal image (figure 3) demonstrates a rather uniform low signal intensity adjacent to the articular cortex of the medial femoral condyle.

Advanced cases may ultimately result in articular collapse, as depicted in image 4. There is an indentation of the articular cortex with low signal intensity marrow edema surrounding it on the T-1 weighted coronal image. There has also been subsequent formation of bone marrow edema in the subjacent medial tibial plateau.
The prognosis for SONK is very much dependent on early diagnosis. If the lesion is small (defined as involving less than 50% of the width of the femoral condyle [2]), non-weight bearing may be sufficient for recovery. Larger lesions may require core decompression, similar to that used in avascular necrosis of the hip. If left untreated, there is the very real possibility of articular collapse and subsequent accelerated degenerative joint disease, with the prospect of knee replacement.
References:
1. Yochum TR, Rowe LJ. Essentials of skeletal radiology. 3rd edition. Baltimore: Williams and Wilkins. 2005.
2. Stoller D. W.: Magnetic Resonance Imaging in Orthopaedics and Sports Medicine, ed 2. Philadelphia, J. B. Lippincott Company 1993.
Dr. Gregerson serves as past president of the American Chiropractic Board of Radiology and is chief radiologist at Gregerson Radiology Consultants, a private consulting practice, www.mychiropracticradiologist.com