Is It a Full-Thickness or a Partial-Thickness Tear of the Rotator Cuff?
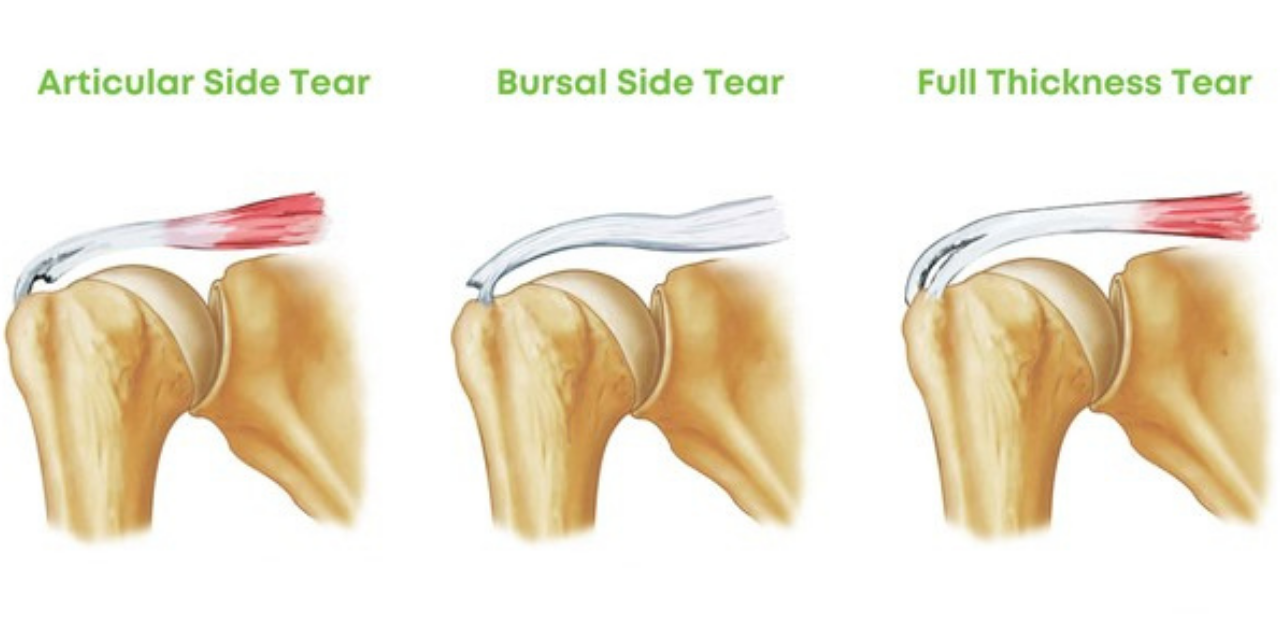
Patients often assume the worst. A recent survey of 1308 participants shared widespread negative concerns about a Rotator Cuff Syndrome (RCS) diagnosis. The results of this survey demonstrate a perception-based fear of shoulder pain. Top responses include psychological distress and uncertainty. These patients are concerned about the historically poor prognosis associated with RCS, usually ending in surgery. (1) There is one question we must all answer for these patients: Is there a full-thickness rotator cuff tear?

Instead of guessing, consider using the best orthopedic tests to identify the proper diagnosis. Once you zero in on the severity of tissue of origin, you can manage these patients more effectively, reducing their fear of “going under the knife.” Making the proper diagnosis between a partial-thickness and full-thickness rotator cuff lesion will make your treatment selection and anticipated prognosis infinitely easier.
Consider using the External Rotation Lag Sign (ERLS) to stop guessing at treatment and prognosis.
The clinician passively flexes the patient’s elbow to 90 degrees with 20 degrees of shoulder abduction with the patient seated. The clinician then passively takes the patient’s shoulder into a position of maximal external rotation. The patient is then instructed to hold that position. The test is positive if the patient cannot maintain this position, as evidenced by retreating into internal rotation. A positive test is fairly specific and sensitive for a full-thickness tear of the supraspinatus tendon.

The ERLS exploits the fact that a muscle with a full-thickness tear has less capacity to work. This test is highly specific and acceptably sensitive for diagnosing a full-thickness tear. Positioning during the test prevents synergistic muscles from compensating for a weak supraspinatus or infraspinatus. Testing the shoulder in an abducted position exploits a weak supraspinatus secondary to a tear. The anterior band of the supraspinatus (most common tear location) is an agonist to external rotation. (2) In the presence of a full-thickness tear, there is less ability to generate joint torque, hence a positive lag sign.
A full-thickness tear will decrease the capacity of a muscle to do work. These muscles will atrophy faster and not regain strength compared to a muscle with a partial thickness tear. (3)
Does nighttime pain mean my patient has a rotator cuff tear?
Between 70-90% of rotator cuff tendinopathy patients report sleep disturbances. (2) However, the degree of nighttime pain has no relevance to the size of the tear. (3) Night-time pain is a key clinical symptom, but still requires a physical exam and history to support the diagnosis of a rotator cuff tear.
Should I perform an MRI to document a rotator cuff tear?
You should consider advanced imaging in the absence of red flags after 4-6 weeks of failed conservative care. These expensive tests are needed to identify the possible need for future care, such as injection or surgery. Fortunately, the ERLS has similar sensitivity and specificity as ultrasound and MRI. Teefey, et al., have reported that the accuracy of US and MRI for diagnosing full-thickness tears is 98% and 100%, respectively. (5)
US and MRI accuracy is only 68% and 63% for partial-thickness rotator cuff tears (5)
If my patient has a full-thickness tear, is surgery an option?
Unfortunately, 82.4% of symptomatic full-thickness rotator cuff tears increased in size over a follow-up period of 6–100 months. (6) Arthroscopic repair of a full-thickness tear of the supraspinatus benefits those who do not respond to our clinical care. (7) Nobody wants to have surgery, but sometimes it can be helpful to prevent chronic pain and disability.
In conclusion, making the differential diagnosis between a partial thickness tear and a full-thickness tear will help you develop the right treatment strategies and give a more accurate prognosis for the condition. ChiroUp subscribers can check out the condition references on Shoulder Anterior Impingement Syndrome and Rotator Cuff Syndrome for the complete list of evaluations and treatment strategies for your next patient with shoulder pain.
References
- Park JY, Chung KT, Yoo MJ. A serial comparison of arthroscopic repairs for partial- and full-thickness rotator cuff tears. Arthroscopy, 2004, 20: 705–711.
- Lehman C, Cuomo F, Kummer FJ, Zuckerman JD. The incidence of full-thickness rotator cuff tears in a large cadaveric population. Bull Hosp Jt Dis. 1995;54:30-1
- Lundgreen K, Lian ØB, Engebretsen L, Scott A. Lower muscle regenerative potential in full-thickness supraspinatus tears compared to partial-thickness tears. Acta orthopaedica. 2013 Dec 1;84(6):565-70.
- Keung WW, Yan LM, Hang YP, Teng LH. The effect of psychological factors on pain, function and quality of life in patients with rotator cuff tendinopathy: A systematic review. Musculoskeletal Science and Practice. 2020 Apr 29:102173.
- Teefey SA, Rubin DA, Middleton WD, et al. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am, 2004, 86-A: 708–716.
- Kim YS, Kim SE, Bae SH, Lee HJ, Jee WH, Park CK. Tear progression of symptomatic full-thickness and partial-thickness rotator cuff tears as measured by repeated MRI. Knee Surgery, Sports Traumatology, Arthroscopy. 2017 Jul;25(7):2073-80.
- Bennett WF. Arthroscopic repair of full-thickness supraspinatus tears (small-to-medium): a prospective study with 2-to 4-year follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003 Mar 1;19(3):249-56.