
The Imaging Features of Fibrous Dysplasia

Fibrous dysplasia has been termed “the great imitator,” although it is one of two entities that have been dubbed with this distinction (the other being Paget’s disease). It has been called this because of its propensity to mimic a multitude of other osseous diseases processes. Fibrous Dysplasia is a benign entity, and, although its appearance may suggest a neoplastic process, it is in fact not neoplastic. Fibrous Dysplasia is a developmental disturbance in cancellous bone maintenance that results in islands of cartilage and spicules of bone in a collagenous matrix. Monostotic and polyostotic forms occur and there are differences in the predilection for sites of involvement and the non-osseous abnormalities that are associated with each.
The lesion usually begins in childhood, generally between the ages of 8 and 14 (1). It will continue to grow throughout the patient’s lifetime. There is no difference in gender predilection, with the exception of the type that is associated with McCune-Albright syndrome, which is almost exclusively found in females.
Skeletal Lesions
The actual skeletal lesions may be similar in both varieties. Variation in the amount of collagen and bone in the matrix of the lesion will determine if it appears lucent, sclerotic or ground glass. The lesion may be surrounded by a thick rind of sclerosis and thus be well defined. Bowing deformities are common in the long bones. A particular deformity that may be noted in the proximal femur is the Shepherd’s crook deformity, in which there is a 90-degree angle that forms between the neck and shaft of the femur. Some lesions may result in the thinning of the endosteal layer of the cortex with the expansion of the medullary cavity. Pathologic fractures are more common with the polyostotic variety, and thus this type may be more prone to symptomatology.
The monostotic type is found more commonly in the proximal femur, ribs, tibia, and skull. Polyostotic Fibrous Dysplasia is commonly found in the femur, skull, tibia, humerus, ribs, fibula radius and ulna. Vertebral involvement is not common; however, when present, it affects the vertebral body and is associated with the polyostotic variety.
MRI Findings
Findings on MRI feature homogenously low signal on the T-1 weighted images (2). The high signal is seen on the T-2 weighted images in 60% of cases, often with mixed signals and a thin rim of sclerosis. Active lesions will enhance with contrast.
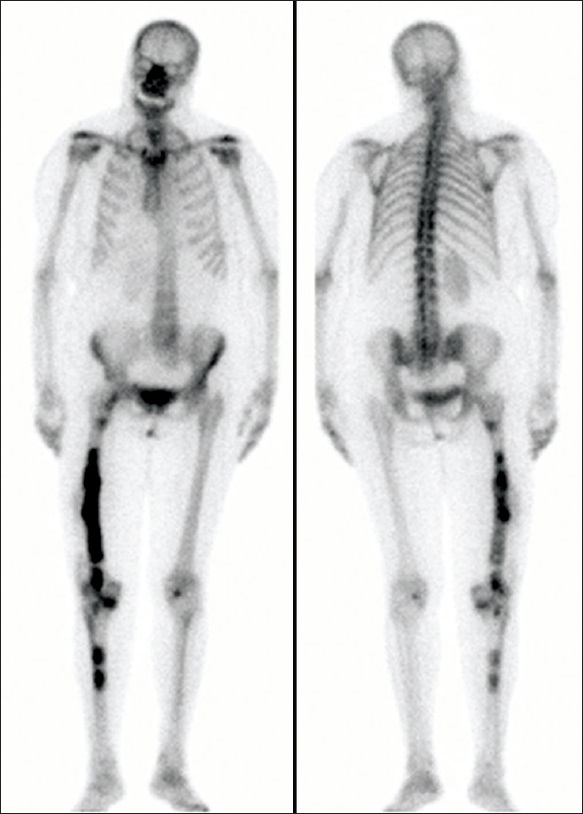
On radionuclide bone scans, there is increased uptake in the majority of the lesion. As lesions become less active, the radiotracer uptake is decreased.
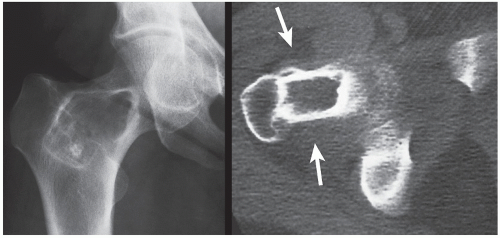
Figure 1 demonstrates a monostotic lesion in the proximal femur. It is well defined with a sclerotic border and is largely lucent. The associated CT scan on the right shows the lesion as lucent without obvious calcification.
In figure 2 there is a polyostotic involvement with lesions in the pelvis and femora. The right femur demonstrates a sclerotic character, while the extensive left femoral lesion and left hemipelvis are lucent, with obvious deformity of the femur.
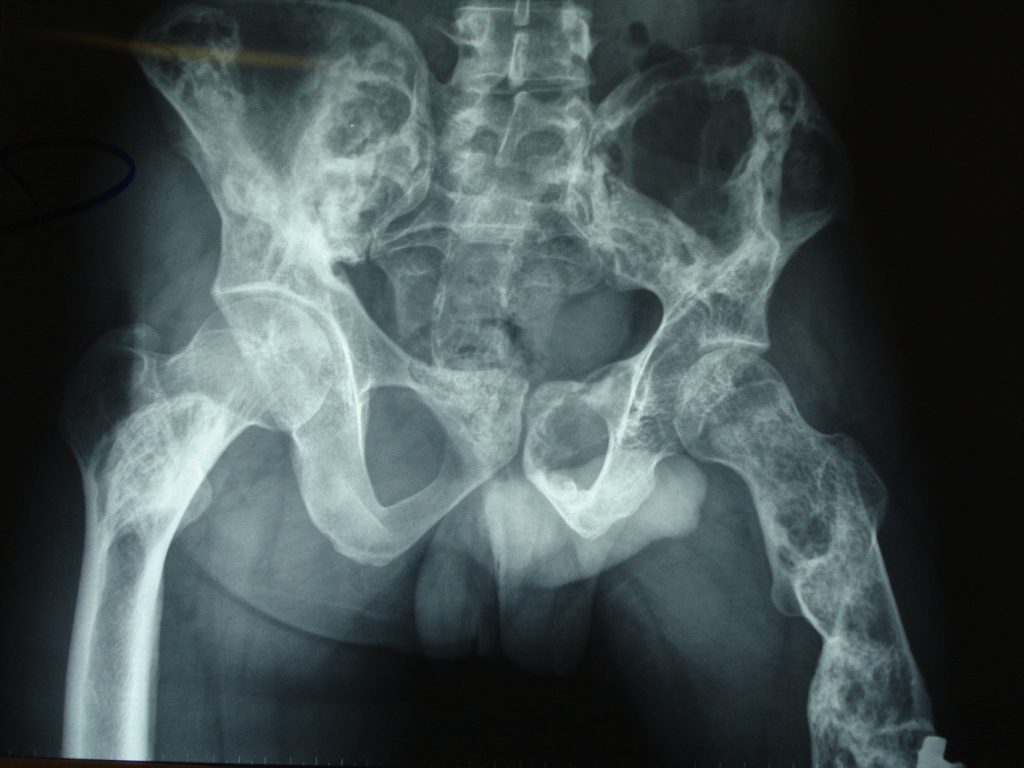
Figure 3 contrasts a plain film radiograph with two MRI pulse sequences of a tibial lesion. The center image is T-1 weighted, revealing a rather uniform low signal intensity lesion. The right-sided images are T-2 weighted and demonstrate a heterogeneous lesion that is largely hyperintense with hypointense foci within the matrix. All images show the well-defined character of the lesion.
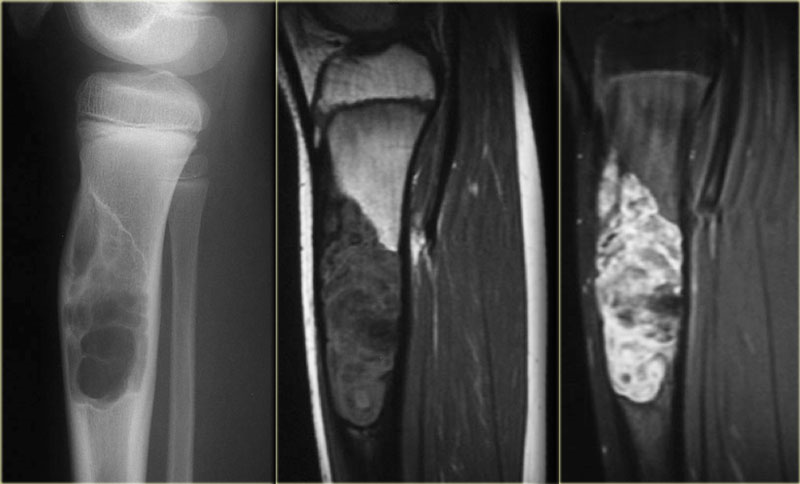
Figure 4 represents a radionuclide bone scan demonstrating polyostotic lesions, with multiple areas of increased uptake in the facial bones, pelvis, femur, and tibia.
As mentioned earlier, although rare, there may be involvement of the spine. On the T-2 weighted images in figure 5, there are foci of high signal intensity within the L4 vertebral body, with osseous expansion.

Fibrous Dysplasia may resemble other benign lesions and have a wildly varying appearance. The generally well-defined character of the lesion, along with a lack of periosteal reaction in an otherwise asymptomatic lesion, may be good clues to its true nature.
References
- Yochum T.R., Rowe L.J.: Essentials of Skeletal Radiology, ed 3. Philadelphia, Lippincott Williams & Wilkins, 2005.
- Stoller D.W.: Magnetic Resonance in Orthopaedics and Sports Medicine, Philadelphia, Lippincott Company 1993.

















