The Imaging of Chondromalacia Patella

The Imaging of Chondromalacia Patella
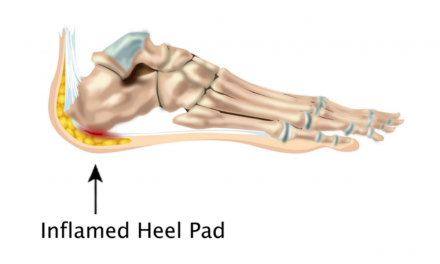
Chondromalacia patella (CP) is a relatively common condition involving the knee that pathologically features the softening of the hyaline cartilage of the patella. Unlike degenerative conditions, however, it tends to involve a younger age group. The condition is slightly more common in females. Typically, there is anterior knee pain on ascending or descending stairs or after kneeling or squatting for long periods of time.
MRI
The imaging findings on plain film x-ray may be few or non-existent. CT arthrography may be useful for imaging purposes once the disease has progressed to actual focal cartilage defect, but is not good at detecting an early change and has the additional disadvantage of being an invasive procedure. MRI, however, is a good modality to show the cartilage degradation that may occur with this condition, even in the initial stages. MRI is uniquely suited to demonstrate the early softening of the hyaline cartilage. In addition, MRI provides excellent visualization of all of the soft tissues of the knee, as well as the osseous structures, and can demonstrate other conditions that may mimic Chondromalacia patella symptomatically, such as Sinding-Larsen-Johansson disease.
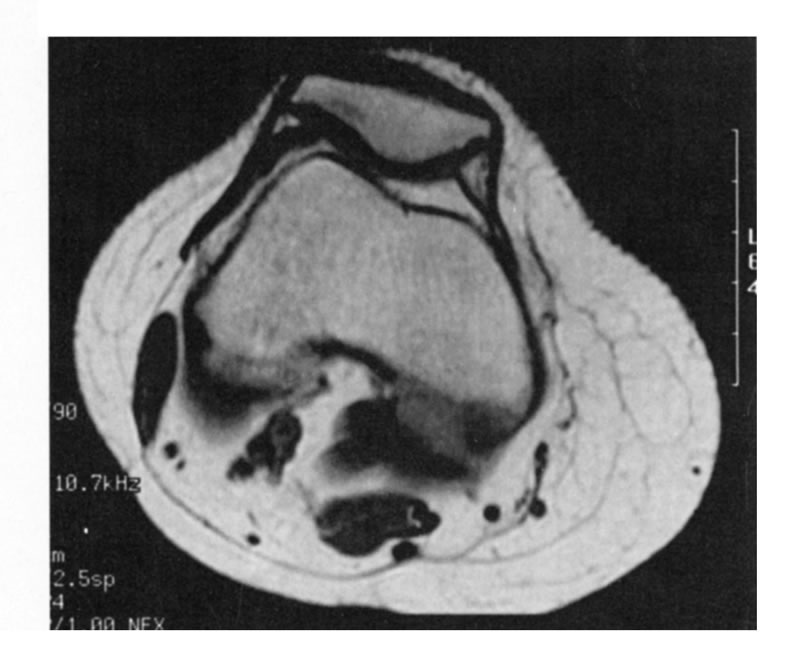
Patellar hyaline cartilage is usually best demonstrated on the axial T-2 or fat suppressed sequences. Abnormality of the cartilage manifests as increased signal intensity on these sequences, compared to normal cartilage.
The grading for CP generally utilizes a I-IV scale 1 with the following MRI criteria:
• Grade I consists of focal areas of increased signal on the fat-suppressed images without cartilage attenuation.
• Grade II manifests as a frayed appearance of the surface of the cartilage with a degree of cartilage swelling.
• Grade III will show partial thickness loss of the cartilage with focal areas of ulcerative change.
• Grade IV shows full thickness cartilage loss with reactive underlying osseous change.
Images
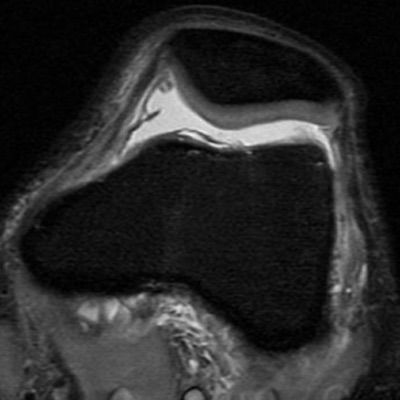
Figure 1 
Figure 2
Fat-suppressed axial images were utilized in the following descriptions of figures 1-6. Figure 1 shows a normal uniform thickness hyaline cartilage. In figure 2 there are focal areas of increased signal within the cartilage, representative of type I change. Figure 3 demonstrates an appearance of increased cartilage thickness at the medial patellar facet with the irregularity of the cartilage surface representing a grade II lesion. In figure 4 there are areas of focal partial thickness cartilage loss corresponding to a grade III lesion. Figure 5 represents large areas of full thickness cartilage loss with adjacent high signal intensity osseous marrow change. Plain film x-rays of this same patient in Fig. 6 and 7 fail to demonstrate the advanced nature of this involvement.
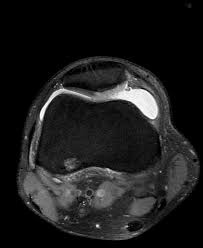
Figure 3 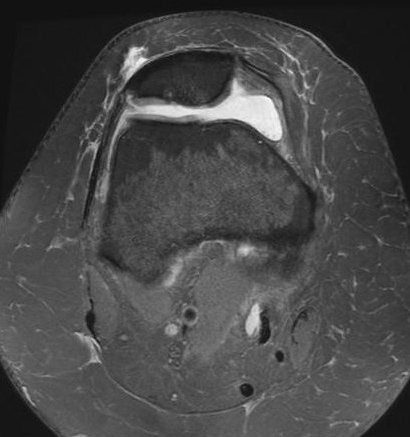
Figure 4 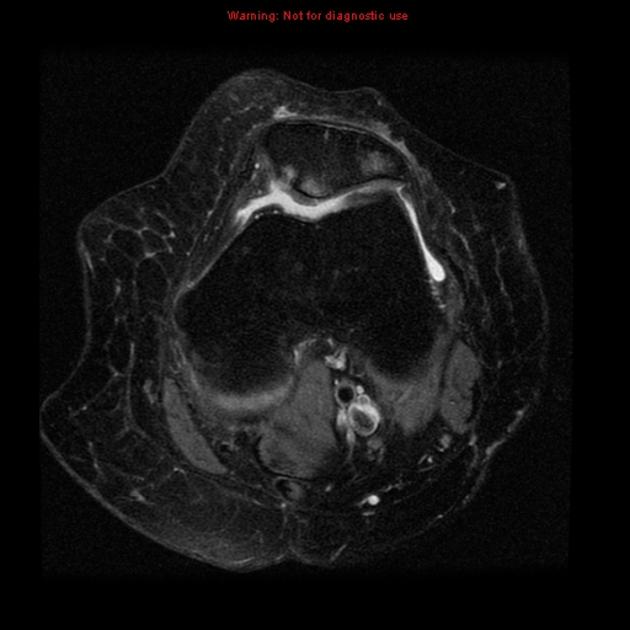
Firugre 5 
Figure 6 
Figure 7
Underlying Factors
Underlying factors that may be associated with Chondromalacia patella include patellar tracking abnormalities. Figure 8 demonstrates a lateral subluxation of the patella, which may result in asymmetrical stress across the patellofemoral articulation and increased pressure on segments of the cartilage. Other predispositions to CP may include pes planus, over-pronation gait syndromes, and obesity.
Conservative care remains the treatment of choice for the majority of cases of CP. Surgical options are available when conservative measures fail. In severe cartilage loss with loose body formation, arthroscopic debridement, as well as articular resurfacing, may be indicated. In extreme cases, patellectomy may be considered.
Treatment
MRI is the modality of choice in effectively demonstrating the severity of involvement in CP, as well as being able to detect early change. This can be done non-invasively and without discomfort to the patient.
References:
1. “Diagnostic Imaging Orthopaedics” Stoller, D. W. et al; Amirsys, Salt
Lake City, UT; 2004.